Sarcoidosis is a disease that occurs as a result of a certain type of inflammation. It can appear in almost any organ of the body, but most often begins in the lungs or lymph nodes.
The cause of sarcoidosis is unknown. The disease can suddenly appear and disappear. In many cases, it develops gradually and causes symptoms that come and go, sometimes throughout a person's life.
As sarcoidosis progresses, microscopic inflammatory foci - granulomas - appear in the affected tissues. In most cases, they disappear spontaneously or with treatment. If the granuloma does not dissolve, a patch of scar tissue forms in its place.
Sarcoidosis was first studied over a century ago by two dermatologists, Hutchinson and Beck. In the beginning, the disease was called "Hutchinson's disease" or "Benier-Beck-Schaumann disease." Dr. Beck then coined the term sarcoidosis, derived from the Greek words for flesh and like, into medical practice. This name describes skin rashes that are often caused by an illness.
Sarcoidosis is a disease that occurs suddenly for no apparent reason. Scientists are considering several hypotheses for its appearance:
- Infectious. This factor is considered as a trigger for the development of the disease. The constant presence of antigens can disrupt the production of inflammatory mediators in genetically predisposed people. As triggers are considered mycobacteria, chlamydia, the causative agent of Lyme disease, bacteria living on the skin and in the intestines; hepatitis C viruses, herpes, cytomegalovirus. In support of this theory, observations are made on the transmission of sarcoidosis from animal to animal in experiment, as well as during organ transplantation in humans.
- Environmental. Granulomas in the lungs can form under the influence of dust from aluminum, barium, beryllium, cobalt, copper, gold, rare earth metals (lanthanides), titanium and zirconium. The risk of illness increases with contact with organic dust, during agricultural work, construction, and working with children. It has been proven to be higher on contact with mold and smoke.
- Heredity. Among family members of a patient with sarcoidosis, the risk of getting sick is several times higher than the average. Several genes responsible for familial cases of the disease have already been identified.
The basis for the development of the disease is a delayed-type hypersensitivity reaction. In the body, the reactions of cellular immunity are suppressed. In the lungs, on the contrary, cellular immunity is activated - the number of alveolar macrophages, which produce inflammatory mediators, increases. Under their action, the lung tissue is damaged, granulomas are formed. Produced big number antibodies. There is evidence of the synthesis of antibodies against their own cells in sarcoidosis.
Who can get sick
Previously, sarcoidosis was considered a rare disease. It is now known that it is chronic illness occurs in many people around the world. Sarcoidosis of the lungs is one of the main causes of pulmonary fibrosis.
Anyone, an adult or a child, can get sick. However, the disease, for an unknown reason, more often affects representatives of the Negroid race, especially women, as well as Scandinavians, Germans, Irish and Puerto Ricans.
Because the disease may be overlooked or misdiagnosed, the exact number of patients with sarcoidosis is unknown. It is believed that the incidence is about 5 - 7 cases per 100 thousand of the population, and the prevalence is from 22 to 47 patients per 100 thousand. Many experts believe that the incidence of the disease is actually higher.
People between the ages of 20 and 40 are more likely to get sick. Sarcoidosis is rare in people under 10 or over 60 years of age. The prevalence of the disease is high in the Scandinavian countries and North America.
The disease usually does not bother the person. Within 2 - 3 years in 60 - 70% of cases, it disappears spontaneously. In a third of patients, irreversible damage to the lung tissue occurs, in 10% the disease becomes chronic. Even with a prolonged course of the disease, patients can lead a normal life. Only in some cases with severe heart damage, nervous system, liver or kidney disease can cause poor outcome.
Sarcoidosis is not a tumor. It is not spread from person to person through household or sexual contact.
It is rather difficult to predict how the disease will develop. It is believed that if the patient is more concerned about general symptoms such as weight loss or malaise, the course of the disease will be milder. If the lungs or skin are affected, a longer and more severe process is likely.
Classification
Diversity clinical manifestations suggests that the disease has several causes. Depending on the localization, such forms of sarcoidosis are distinguished:
- classic with a predominance of lesions of the lungs and intrathoracic lymph nodes;
- with a predominance of damage to other organs;
- generalized (many organs and systems are affected).
According to the characteristics of the flow, the following options are distinguished:
- with an acute onset (Löfgren's syndrome, Heerfordt-Waldenstrom);
- with a gradual onset and chronic course;
- relapse;
- sarcoidosis in children under 6 years of age;
- not amenable to treatment (refractory).
Depending on the X-ray picture of organ damage chest distinguish the stages of the disease:
- There are no changes (5% of cases).
- Lymph node pathology without lung involvement (50% of cases).
- Damage to both lymph nodes and lungs (30% of cases).
- Only the lungs are affected (15% of cases).
- Irreversible pulmonary fibrosis (20% of cases).
Sequential staging is uncommon for pulmonary sarcoidosis. Stage 1 indicates only the absence of changes in the organs of the chest, but does not exclude sarcoidosis of other localizations.
Possible complications:
- stenosis (irreversible narrowing of the lumen) of the bronchus;
- atelectasis (collapse) of the area of the lung;
- pulmonary insufficiency;
- cardiopulmonary failure.
In severe cases, the process in the lungs can end with the formation of pneumosclerosis, (swelling) of the lungs, fibrosis (compaction) of the roots.
According to the International Classification of Diseases, sarcoidosis refers to diseases of the blood, hematopoietic organs and certain immunological disorders.
Sarcoidosis: symptoms
The first manifestations of sarcoidosis can be and. The disease can begin suddenly with the appearance of a skin rash. The patient may be disturbed by red spots (erythema nodosum) on the face, skin of the legs and forearms, as well as eye inflammation.
Sarcoidosis of the skin
In some cases, the symptoms of sarcoidosis are more general character... This is weight loss, fatigue, night sweats, fever, or just general malaise.
In addition to the lungs and lymph nodes, the liver, skin, heart, nervous system and kidneys are often affected. Patients may have general symptoms of the disease, only signs of damage to individual organs, or not complain about anything at all. The manifestations of the disease are detected by X-ray of the lungs. In addition, an increase in the salivary, lacrimal glands is determined. Cysts - rounded hollow formations can form in the bone tissue.
The most common development is sarcoidosis of the lungs. 90% of patients with this diagnosis have complaints of shortness of breath and cough, dry or with phlegm. Sometimes there is pain and a feeling of stuffiness in the chest. It is believed that the process in the lungs begins with inflammation of the respiratory vesicles -. Alveolitis either disappears spontaneously or leads to the formation of granulomas. The formation of scar tissue at the site of inflammation leads to impaired lung function.
The eyes are affected in about a third of patients, especially in children. Almost all parts of the organ of vision are affected - the eyelids, cornea, sclera, retina and lens. As a result, there is redness of the eyes, watery eyes, and sometimes loss of vision.
Sarcoidosis of the skin appears as small raised spots on the skin of the face that are reddish or even purple in color. The skin on the limbs and gluteal regions is also involved. This symptom is recorded in 20% of patients and requires a biopsy.
Another cutaneous manifestation of sarcoidosis is erythema nodosum. It has a reactive character, that is, it is nonspecific and arises in response to an inflammatory response. These are painful nodules on the skin of the legs, less often on the face and in other areas of the body, initially red in color, then yellowing. In this case, pain and swelling of the ankle, elbow, wrist joints, and hands often occurs. These are signs of arthritis.

Erythema nodosum
In some patients, sarcoidosis affects the nervous system. One of the signs of this is paralysis of the facial nerve. Neurosarcoidosis is manifested by a feeling of heaviness in the back of the head, headache, impairment of memory for recent events, weakness in the limbs. With the formation of large foci, convulsive seizures may appear.
Sometimes the heart is involved with the development of rhythm disturbances, heart failure. Many sufferers suffer from depression.
The spleen may enlarge. Its defeat is accompanied by bleeding, a tendency to frequent infectious diseases. Less commonly, the ENT organs, the oral cavity, the genitourinary system, and the digestive system are affected.
All of these signs can appear and disappear over the years.
Diagnostics
Sarcoidosis affects many organs, therefore, it may require the help of different specialists to diagnose and treat it. It is better for patients to be treated by a pulmonologist or in a specialized medical center dealing with the problems of this disease. It is often necessary to consult a cardiologist, rheumatologist, dermatologist, neurologist, ophthalmologist. Until 2003, all patients with sarcoidosis were seen by a phthisiatrician, and most of them received anti-tuberculosis therapy. This practice should not be used now.
The preliminary diagnosis is based on the data of the following research methods:
- analysis of the history of the disease;
- inspection;
- laboratory tests;
The diagnosis of sarcoidosis requires the exclusion of similar diseases such as:
- beryllium (damage to the respiratory system during prolonged contact with the metal beryllium);
- rheumatoid arthritis;
- rheumatism;
- malignant tumor of the lymph nodes (lymphoma).
There are no specific changes in analyzes and instrumental studies for this disease. The patient is assigned general and biochemical blood tests, X-ray of the lungs,.
Chest x-rays are useful for detecting changes in the lungs as well as mediastinal lymph nodes. IN Lately it is often supplemented with computed tomography of the respiratory system. Multispiral computed tomography data are of high diagnostic value. Magnetic resonance imaging is used to diagnose neurosarcoidosis and heart disease.
The patient often has impaired function of external respiration, in particular, the vital capacity of the lungs decreases. This is due to a decrease in the respiratory surface of the alveoli as a result of inflammatory and cicatricial changes in the lung tissue.
In a blood test, signs of inflammation can be determined: an increase in the number of leukocytes and ESR. When the spleen is damaged, the number of platelets decreases. The content of gamma globulins and calcium increases. In case of impaired liver function, an increase in the concentration of bilirubin, aminotransferases, alkaline phosphatase is possible. To determine kidney function, blood creatinine and urea nitrogen are determined. In some patients, an in-depth study determines an increase in the level of angiotensin-converting enzyme, which is secreted by granuloma cells.
A general urine test and an electrocardiogram are performed. In case of cardiac arrhythmias, 24-hour Holter ECG monitoring is indicated. If the spleen is enlarged, the patient is prescribed magnetic resonance imaging or computed tomography, where rather specific rounded foci are detected.
For the differential diagnosis of sarcoidosis, and are used. The number of different cells is determined, reflecting the inflammatory and immune processes in the lungs. In sarcoidosis, a large number of leukocytes are determined. During bronchoscopy, a biopsy is performed - the removal of a small piece of lung tissue. With its microscopic analysis, the diagnosis of "sarcoidosis of the lungs" is finally confirmed.
A radioactive scan can be used to identify all foci of sarcoidosis in the body. chemical element gallium. The drug is administered intravenously and accumulates in areas of inflammation of any origin. After 2 days, the patient is scanned with a special device. Areas of accumulation of gallium indicate areas of inflamed tissue. The disadvantage of this method is the indiscriminate binding of the isotope in the focus of inflammation of any nature, and not only in sarcoidosis.
One of the promising research methods is transesophageal ultrasound of the intrathoracic lymph nodes with simultaneous biopsy.
Shown are tuberculin skin tests and examination by an ophthalmologist.
In severe cases, video-assisted thoracoscopy is shown - examination of the pleural cavity using endoscopic techniques and taking a biopsy material. Open surgery is extremely rare.
Sarcoidosis: Treatment
Many patients do not need treatment for sarcoidosis. Signs of the disease often disappear spontaneously.
The main goal of treatment is to preserve the function of the lungs and other affected organs. For this, glucocorticoids are used, primarily prednisolone. If the patient has fibrous (cicatricial) changes in the lungs, then they will not disappear.
Hormone treatment is initiated when symptoms of severe damage to the lungs, heart, eyes, nervous system, or internal organs are present. Taking prednisolone usually improves the condition quickly. However, after the hormones are canceled, the symptoms of the disease may return. Therefore, sometimes several years of treatment are required, which are started when the disease recurs or for its prevention.
To make timely adjustments to your treatment, it is important to visit your doctor regularly.
Long-term use of corticosteroids can cause side effects:
- mood swings;
- swelling;
- weight gain;
- hypertension;
- diabetes;
- increased appetite;
- stomach pain;
- pathological fractures;
- acne and others.
However, with the administration of low doses of hormones, the benefits of treatment are greater than their potential adverse effects.
As part of complex therapy, chloroquine, methotrexate, alpha-tocopherol, pentoxifylline can be prescribed. Efferent methods of treatment are indicated, for example, plasmapheresis.
In case of sarcoidosis that is difficult to treat with hormones, as well as in case of damage to the nervous system, it is recommended to prescribe the biological drug infliximab (Remicade).
Erythema nodosum is not an indication for the appointment of hormones. It goes away under the influence of non-steroidal anti-inflammatory drugs.
For limited skin lesions, glucocorticoid creams can be used. The widespread process requires systemic hormone therapy.
Many people with sarcoidosis lead normal lives. They are advised to quit smoking and see a doctor regularly. Women can carry and give birth to a healthy baby. Difficulties with conception occur only in older women with a severe form of the disease.
In some patients, there are indications for determining the disability group. This, in particular, respiratory failure, cor pulmonale, damage to the eyes, nervous system, kidneys, as well as long-term ineffective treatment with hormones.
Sarcoidosis of the lungs is a benign pathology characterized by the formation of inflammatory foci (granulomas) in the lung tissue, resembling nodules in shape. The disease belongs to the category of systemic, the whole organism can feel the negative. However, more often, the lesion affects the lungs, lymph nodes.
There are no age, territorial restrictions, women and men are equally susceptible. True, the female body is characterized by an additional relapse, in the interval between 40-60 years.
The peak falls on the age range of 25-49 years. Respiratory system - intrathoracic lymph nodes (HLN), lungs, “favorite target” for sarcoidosis attacks. In addition, the list of organs capable of being attacked by granulomas will be supplemented by:
- eyes
- liver
- skin covering
- joints
- bones
- spleen
- kidneys
Growing up, granulomatous accumulations merge, forming multiple inflammatory foci. Such sarcoid granulomas seriously harm the functionality of the organ in which they are localized. The disease develops, negative symptoms arise, fibrotic changes are likely in the affected area.
As you can see, the list is extensive, the systemic nature of the pathology is obvious, therefore, therapy is prescribed and corrected exclusively by a pulmonologist, who will competently assess the severity of the lesion, and prescribe the correct, full-fledged treatment.
What are the causes of the disease
The etiology has not yet been formally formulated. There is no reliable information confirming the nature of the origin. There are hypotheses that the following risk factors give impulse impulse:
- infectious
- genetic
- professional
- domestic
- medicinal
Let's dwell in more detail on each of the above factors.
Infectious hypothesis based on the fact that some pathogenic microorganisms provoke the onset of the disease. The list of probable pathogens includes bacteria, viruses, fungal microorganisms:
- Mycobacterium tuberculosis - tuberculosis occurs
- Chlamydia pneumoniae - the causative agent of chlamydia
- Helicobacter pylori - gastritis develops,
- Viruses - hepatitis C, herpes, rubella, adenovirus infection
- Mycoses
- Spirochetes
- Histoplasma capsulatum - provokes histoplasmosis
There are plenty of provocative bacterial microorganisms that affect the development of the disease, however, it was not possible to identify a single infectious agent that was guaranteed to indicate the disease.
Genetic factor are still considered exclusively theoretical, since there are no specific data on changes at the gene level that affect the development of pathology.
Professional- there is a tendency for sarcoidosis to affect workers in the following professions:
- postal workers
- firefighters
- miners
- librarians
- farmers
- doctors
- chemical workers
The main risks are dust, polluted air, fertile soil for the development of pathology.
In addition, dust particles of metals are involved in the formation of foci of granulomatous accumulations:
- beryllium
- cobalt
- aluminum
- zirconium
Among household reasons, indirectly affecting the course of the disease include molds that penetrate inside along with the air.
Drug hypothesis the influence of certain drugs on the progression of the disease is based on the data that prolonged use of certain drugs increases the inflammatory process.
Sarcoidosis of the lungs - the pathology is not contagious, there is no danger of contagiousness.
Classification of sarcoidosis
There are four characteristic stages:
- Zero - painful symptoms are absent, X-ray does not reveal pathological disorders.
- First, the lung tissue is not affected, but a slight change in the size of the intrathoracic lymph nodes is noted. The pulmonary lymph nodes, called bronchopulmonary, become inflamed, asymmetrically increasing. Other intrathoracic lymph nodes- paratracheal, bifurcation, tracheobronchial, less often suffer from a pathological process.
- Number two is called mediastinal - the attack spreads to the lymph nodes. Focal darkening of the lung tissue is classified into small, medium, large, when the size of the granulomas is comparable to small neoplasms. The patient has difficulty breathing, there is a tangible pain in the chest. The mediastinal form is “fixed” by fluorography, however, the biopsy procedure - morphological confirmation of lymphoid cells can clearly state the presence of sarcoidosis.
- Third, there are tangible changes in the lung tissue.
- The fourth is fibrosis, an irreversible process of replacement with connective tissue occurs, with the formation of scars. Pathological disorders lead to increasing respiratory failure, the likelihood of critical consequences for the body increases.
In addition to the stages described above, sarcoidosis is classified according to localization, the nature of the course, the rate of growth of pathological changes.
Localization:
- intrathoracic lymph nodes
- lungs
- The lymph nodes
- respiratory system
- numerous lesions of organs, body systems
The nature of the flow
phases active, stabilization, decay
Slew rate
- chronic
- abortive
- growing
- delayed
Clinical picture
The disease is prone to self-regression, has the ability to “disappear” without medication. Not every manifestation is accompanied by therapeutic intervention.
If the diagnosis is established, but medical prescriptions were not followed, then it is extremely important for the patient to adhere to the following recommendations for preventive purposes:
- systematically monitor the work and rest regime
- exclude any
- avoid stressful situations, reduce psychological stress
- increase the proportion of vitamins in your daily diet
After three months after the initial diagnosis, a secondary ultrasound is performed, on the basis of which a verdict on further treatment is made.
As the disease develops, pathological changes in the lungs can go through three stages:
- Stage one, initial - the formation of inflammatory granulomatous accumulations, accurate diagnosis is problematic.
- Stage two - the formation of new foci of inflammation stops. The increase in the size of the "old" formed granuloma slows down. Clinical symptoms remain, but the patient's condition is not seriously worsened.
- The third stage - the disease develops slowly, the accumulation of granulomatous cells increases. Foci of necrosis are formed, the symptomatic picture expands due to pathological signs from other organs that were previously in health.
There is a list of general nonspecific symptoms, the presence of which does not indicate a lesion, however, the presence of such manifestations is the primary "bell" of an approaching sarcoidosis.
The initial symptoms of the disease include:
- Persistent fatigue and weakness are the most popular complaints among nonspecific symptoms. A systematic state of weakness is an early bell in the body, the appearance of which is possible long before a visit to a doctor. Weakening, capable of overcoming the patient for a long time (months), before the manifestation of other pathological signs.
- Weight loss is noted along with the characteristic signs at the stage when the diagnosis is completed. The decrease in body weight is due to: difficult to treat inflammatory phenomena "dominating" in the lungs, metabolic disorders. The body is unable to fully assimilate nutrients.
- Fever is an "infrequent guest", the temperature rise is moderate. A similar symptom is typical for granulomas of the eyes, parotid lymph nodes.
- Inflammation of the lymph nodes - the cervical lymph nodes are especially affected. The increase in size is due to an increase in the outflow of lymph, the growth of granulomas.
- Poor appetite
- Constant anxiety and worry for no reason
- Sleep disturbance
- Rapid fatigue
Clinical presentation for stages of sarcoidosis:
The initial, first stage is characterized by the presence of the above-mentioned, general, nonspecific signs of sarcoidosis.
In addition, the patient is worried about pain in the chest area, aching joints, erythema nodosum, and weakness.
Feels drowsy during the day, depression. Stage two, mediastinal, is characterized by an extended symptomatic pattern:
- dyspnea
- cough
- scattered dry wheezing
- chest pains, episodic
The third is pulmonary, there is a combination of the first two stages.
The situation is aggravated by increased cough with phlegm, the pain increases, arthralgia occurs.
At this stage, a number of complications are possible:
- respiratory distress
- emphysema
- pneumosclerosis of the lung tissue
- enlargement and expansion of the right atrium, circulatory failure
- enlarged liver
- central nervous system damage
- Problems visual organs, in the absence of adequate treatment, up to complete loss of vision
- a wide range of skin pathologies
How is sarcoidosis diagnosed?
List of conducted surveys:
- x-ray
- high resolution computed tomography
- Ultrasound of potentially affected organs: heart, kidneys, thyroid, liver, small pelvis
- biopsy - material (biopsy) is taken from the affected organ
- recording and analysis of the forced expiratory flow-volume curve
- electrocardiogram
- cytomorphological analysis of biopsy - material taken during the biopsy procedure, mediastinoscopy, transthoracic puncture
In sarcoidosis, the information content of the study of the liver, nervous system, heart muscle, increases in the case of magnetic resonance imaging. The fact of the defeat is confirmed by scanning with technetium, gallium.
How is sarcoidosis of the lungs treated?
Since the disease is inherent in the ability to independently regress, the patient is dynamically observed by a pulmonologist for six months. This time interval is required to accurately determine the directional vector of a specific therapy.
If the patient does not have any breathing problems, is absent, the patient does not suffer from shortness of breath, then there is no need for immediate medical intervention by a doctor.
In case of a satisfactory condition, and even minor pathological disorders of the lung tissue, the patient continues to receive exclusively medical advice.
Such therapeutic restraint is due to the ability of granulomas to self-dissolve over time. There is a chance of recovery without medication.
Severe forms of the disease require an obligatory adequate therapeutic intervention, since the risk component is high.
Serious complications, including death, are possible. The indications are: a long-term progressive inflammatory process, a generalized form of sarcoidosis, when the granulomatous lesion has spread to many organs.
Among the medical prescriptions that prescribe a long (from eight months) course of taking drugs are:
- Prednisolone - a specific dosage is prescribed, and further adjusted by the doctor. In case of poor tolerance of the drug, side undesirable manifestations, the treatment regimen is changed, prescribing glucocorticoid drugs, taken two days later.
- Immunosuppressants
- Antioxidants
- Anti-inflammatory drugs - Indomethacin, Nimesulide
- Potassium supplements
It happens that it is required to combine therapeutic regimens: steroid drugs with non-steroidal anti-inflammatory drugs.
The chosen method of treatment is influenced by: the nature, degree of progression, the severity of the disease.
The course, diagnostics of the current state, is monitored by a phthisiatrician. Under a favorable scenario, the patient will have to be registered for one and a half to two years, and in case of complications, the disease will "stretch" for up to five years.
Diet
Close attention is required to pay attention to the nutritious diet. There is no special profile menu, but it is recommended to adhere to general nutritional recommendations. Eat foods that do not provoke an increase in the inflammatory process.
Salt intake should be limited, increase the proportion of protein products in the diet. Provide the body the required amount minerals, especially zinc, silicon dioxide, manganese. Diversify your diet with foods that strengthen the immune system:
- walnuts
- seaweed
- grenades
- chokeberry
- sea buckthorn
- oatmeal
- gooseberry
- legumes
- basil
- black currant
- vegetable oils
- sea fish
- lean meat
Limit to a minimum, or better exclude: sugar, flour products, cheeses, dairy products. No fried food, only boiled.
Folk remedies
You should not get carried away with treatment at home, such independence can cause a deterioration in the patient's well-being. a secondary measure, permissible only in the early stages, after obligatory agreement with a pulmonologist.
Prophylaxis
Since the etiology of the problem remains "vague", there are no special preventive measures regarding sarcoidosis, however, general recommendations must be adhered to:
- become a supporter of a healthy lifestyle
- Do not smoke
- avoid contact with toxic volatile substances, chemicals, dust, dirt - detrimental to lung health
- full sleep
- more outdoors
- exclude calcium-containing foods
The lymphatic system. The lymph nodes most commonly affected by sarcoidosis belong to the hilar and paratracheal groups. Of the superficial lymph nodes, the right prescaled group is most often affected, but damage to any superficial nodes, for example, epitrochlear ones, can be found. Lymph nodes affected by sarcoidosis are a convenient target for biopsy.
Eyes. Eye symptoms occur in patients with sarcoidosis, sometimes up to 25% of cases. The eyes should be examined in all cases of sarcoidosis, preferably with a slit lamp for non-severe, asymptomatic lesions. Uveitis is the most common symptomatic ocular disorder. It develops acutely, with pain in the eyes and fog in front of the eyes, in about Uz cases, while the rest have chronic forms that develop gradually. Conjunctivitis, sometimes phlyctenular, may also occur, especially in the early stages of sarcoidosis. If a tubercle forms, a biopsy of the conjunctiva can be performed, which can histologically confirm the diagnosis. Retinal lesions have recently been discovered. Keratoconjunctivitis dry is expressed in dry eyes, sometimes it can be combined with simultaneous damage to the salivary glands. An increase in the lacrimal glands is possible.
Leather. The most common cutaneous manifestation of sarcoidosis is erythema nodosum, which in severe cases may be accompanied by prolonged fever. Maculopapular eruptions, subcutaneous nodules, plaques, and post-frostbite lupus are other detectable changes. In rare cases, old scars may be infiltrated with sarcoid tissue. A clinical study of a patient with suspected sarcoidosis should include an examination of the existing post-traumatic, postoperative and post-vaccination scars to detect their blanching, which confirms the presence of infiltration. Women appear to be more prone to developing chronic skin lesions.
The gastrointestinal tract. The defeat of the salivary glands and liver is well known; involvement of the pancreas and gastrointestinal tract is rare. There is no evidence that classic Crohn's disease is a manifestation of sarcoidosis. The Kveim test was negative in a series of cases that met the criteria for Crohn's disease. The small and large intestines and stomach appear to be very rarely affected. In one of our cases with a pathological formation in the right iliac region, the granulomatous nature of which was proven and which occupied the terminal part of the ileum and the ascending intestine, there was a positive Kveim test with two different substances. In another case, mesenteric lymphadenopathy, other signs of polysystemic lesions and a positive Kveim test were noted.
Liver changes, although frequent as confirmed by biopsy data, usually do not produce symptoms. When the liver is significantly enlarged, abdominal discomfort may occur to a greater or lesser extent. Severe liver dysfunctions with sarcoidosis are rare. Uveo-parotid fever. Uveo-parotid fever was described by Heerfordt in 1909 as a febrile illness characterized by uveitis and swelling of the parotid salivary glands, often accompanied by paralysis of the facial nerve. Initially regarded as a mild form of tuberculosis, uveo-parotid fever is now considered one of the curious combinations of organ damage that can occur in sarcoidosis. The enlargement of the parotid salivary glands is bilateral in more than half of the cases, and can be mistaken for mumps. In contrast to mumps, swollen salivary glands are painless. The enlargement of other salivary and lacrimal glands can sometimes accompany uveo-parotid syndrome.
Hematopoietic system. Spleen enlargement in sarcoidosis is a relatively common manifestation that is usually asymptomatic. Very large magnifications can cause abdominal discomfort. Spontaneous rupture of the spleen has been described. The combination of an enlarged spleen with hypersplenism is relatively rare. Hemolytic anemia has also been described.
Nervous and endocrine systems. When the nervous system is affected by sarcoidosis, be it infiltration or sarcoid deposits, various clinical pictures appear. These include peripheral neuritis, meningitis, meningoencephalitis, intrathecal processes, and damage to the pituitary gland. There are few reports of sarcoidosis in the nervous system; treatment is often ineffective. We observed 2 patients with meningoencephalitis. The lethal outcome occurred despite taking high doses of corticosteroids, and fresh granulomas were detected at autopsy. Another patient with a pronounced lesion of the meningeal membranes came out of a coma during treatment with prednisolone and then his condition remained satisfactory with the use of maintenance doses.
Sarcoidosis involvement of the posterior lobe of the pituitary gland or hypothalamic region may cause the development of diabetes insipidus... Sarcoidosis rarely affects the anterior pituitary gland or other endocrine glands to the extent that it causes dysfunction.
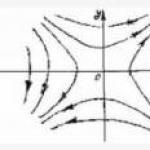
The skeletal system. The most common bone lesions in sarcoidosis are changes in the terminal phalanges of the fingers and toes, although the proximal bones of the extremities are sometimes involved in severe cases. Radiographically, the most typical manifestation of skeletal changes is protruding bone cysts (Fig. 30), first noticed by Kreibich (1904), and later studied in detail by Jungling, but sometimes there is diffuse infiltration of the terminal phalanges, as well as destruction of the cortical and medullary parts of the bone. Bone lesions do not respond to corticosteroid treatment.
Fig. 30. Sarcoidosis. Cystic osteitis (noticeable swelling of soft tissues).
In the Edinburgh Series, bone lesions were observed in only 3% of cases.
Subcutaneous lumps of several fingers or thumbs are often associated with bone damage, which increases the dysfunctions caused by changes in the terminal phalanges. X-ray changes in bone usually do not occur without clinical signs pathology
fingers. In contrast to bone cysts, subcutaneous lumps usually respond to corticosteroid therapy. There are often coexisting cutaneous sarcoids.
As a rule, there is no relationship between the calcium metabolism disorder, defined in some cases of sarcoidosis, and the incidence of bone lesions in this disease.
Sarcoid granulomas can occur in skeletal muscle, most commonly affecting the pectoralis muscle, the muscles of the upper limb, and the calf muscles. Muscle lesions usually do not give symptoms, but in exceptional cases there may be pain, muscle weakness, atrophy, or even pseudohypertrophy. Only in very rare cases is it possible to probe the nodules in the muscles; they are usually found in tendon sheaths.
Regardless of erythema nodosum, "sarcoid arthritis" has been described. However, in most cases, sarcoid polyarthralgia is simply one symptom of erythema nodosum syndrome.
Genitourinary system. Sarcoidosis can affect the kidney in two ways, each of which causes varying degrees of functional impairment. It is possible either the introduction of sarcoid granulomas into the organ, or calcium deposition in and around the tubules of the kidneys (nephrocalcinosis), which is secondary to hypercalcemia or, more often, hypercalciuria. Calcium metabolic disorders in sarcoidosis are caused by an unexplained increase in vitamin D sensitivity, which leads to increased absorption of calcium from the intestine. The importance of corticosteroid therapy in preventing (or reversing) this phenomenon is well known. Insolation has been found to increase the degree of hypercalcemia, and it appears that hypercalcemia in sarcoidosis occurs more frequently in warmer countries with more solar radiation. The pathology is manifested by fatigue, muscle weakness, thirst, polyuria, vomiting, and constipation. Excess calcium deposits can occur in the kidneys, cornea, and subcutaneous tissue. Renal biopsy is warranted if direct renal involvement by sarcoidosis is suspected.
The cardiovascular system. Damage to the cardiovascular system can occur in two forms. Severe pulmonary fibrosis can lead to the development of cor pulmonale and congestive heart failure; true myocardial damage by sarcoidosis can lead to conduction disturbances and the same insufficiency with congestion, as well as to sudden death.
Sarcoidosis Also called sarcoid, is a disease involving abnormal accumulations of inflammatory cells (granulomas) that can form nodules in various organs. Granulomas are most commonly found in the lungs or associated lymph nodes, but any organ can be affected. Sarcoidosis appears to be caused by an immune response to an infection or some other trigger (a so-called antigen that can come from environment), which continues even after the primary infection or other antigen is cleared from the body. In most cases, it heals without medical intervention, but in some cases it causes long-term effects or becomes life-threatening and requires medical attention, most often with medication. 1 alpha, 25 (OH) 2 vitamin D3 is the main cause high level calcium in the blood in sarcoidosis and is produced in excess by sarcoid granulomas. Interferon gamma, produced by activated macrophages and lymphocytes, plays a significant role in the synthesis of 1 alpha, 25 (OH) 2 vitamin D3.
... described the same skin changes, but not associated with frostbite. In a number of works in 1914-1917. Schaumann showed the systemic nature of this disease. (Beck, benign lymphogranulomatosis, benign granuloma) In 1889 Besnier described skin changes localized ...Treatment is usually designed to relieve symptoms and thus does not directly change the course of the disease. This treatment usually consists of anti-inflammatory drugs such as ibuprofen or aspirin. When the condition develops to the point where it is progressive and / or life-threatening, treatment most often includes steroids such as prednisone or prednisolone. In addition, drugs that are most commonly used to treat cancer and suppress the immune system, such as methotrexate, azathioprine, and leflunomide, can be used. The average mortality rate is less than 5% in untreated cases.
In the United States, the disease most commonly affects people of North European (especially Scandinavian or Icelandic) or African / African American descent between the ages of 20-29, although people of any race or age group can be affected. Japan has a lower prevalence of sarcoidosis than the United States, although these people tend to have more aggressive disease and often have heart disease. The Japanese have a peak incidence at a different age - 25-40 years. The disease develops about 2 times more often in women, in whom it most often takes a more aggressive course. Sarcoid in developing countries is often misdiagnosed as tuberculosis because its symptoms often resemble tuberculosis.
Signs and symptoms
Sarcoidosis is a systemic inflammatory disease that can affect any organ, although it can be asymptomatic and is discovered incidentally in about 5% of cases. Typical symptoms are usually vague and include fatigue (not relieved by sleep; present in 66% of cases), weight loss, lack of energy, joint pain and pain (which occurs in about 70% of cases), arthritis (14-38% of individuals ), dry eyes, knee swelling, blurred vision, shortness of breath, dry, hacking cough, or skin damage. More rarely, people may cough up blood. Skin symptoms range from rashes and nodules (small bumps) to erythema, granuloma annulus, or lupus erythematosus. Sarcoidosis and cancer can mimic each other, making it difficult to differentiate.
The combination of erythema nodosum, bilateral hilar lymphadenopathy, and joint pain is called Löfgren's syndrome, which has a relatively good prognosis. This form of the disease is much more common in Scandinavian patients.
Airways
Lung localization is considered the most common manifestation of sarcoidosis today. At least 90% of those affected experience lung involvement. In general, in almost 50% of cases, permanent pulmonary disorders develop and in 5-15% - progressive fibrosis of the pulmonary parenchyma. Sarcoidosis of the lungs is primarily an interstitial lung disease in which the inflammatory process involves the alveoli, bronchi, and small blood vessels. Physical examination in acute and subacute cases usually shows dry wheezing. At least 5% of people will suffer from pulmonary arterial hypertension. Less commonly, there may be violations in the upper respiratory tract (including the larynx, pharynx, paranasal sinuses), which occurs in 5-10% of cases.
Sarcoidosis of the lungs can be divided into four stages. Stage 0 - no intrathoracic involvement. Stage I - bilateral hilar lymph nodes. Stage II - pulmonary parenchyma. Stage III - pulmonary infiltrates with fibrosis. Stage IV - end-stage lung disease with pulmonary fibrosis and void formation.
Leather
The disease affects the skin in 9-37% of individuals. After the lungs, the skin is the second most frequently affected organ. Among the most common skin lesions are erythema nodosum, plaques, maculopapular eruptions, lupus fever, and subcutaneous nodules. Treatment is not required as lesions usually resolve spontaneously within 2-4 weeks. Although it can spoil the appearance, cutaneous sarcoidosis rarely causes serious problems. Sarcoidosis of the scalp manifests as diffuse or focal hair loss.
Eyes
Eye involvement occurs in about 10-90% of cases. Ophthalmic manifestations include uveitis, uveoparotitis, and retinal inflammation, which can lead to loss of visual acuity or blindness. The most common manifestation of ophthalmic sarcoidosis is uveitis. The combination of anterior uveitis, mumps, cranial nerve palsy VII and fever is called uveoparotid fever or Heerford's syndrome. The development of a nodule in the sclera associated with sarcoidosis has been observed.
A heart
The prevalence of cardiac involvement in this disorder varies and varies greatly by race. For example, in Japan, more than 25% of people with sarcoidosis experience symptomatic cardiac involvement, while in the United States and Europe, only about 5% of cases with cardiac involvement. In autopsies in the United States, a heart rate of about 20-30% was found, while in Japan it was 60%. The manifestations of cardiac sarcoidosis can range from asymptomatic conduction abnormalities to fatal ventricular arrhythmias. Conduction abnormalities are most commonly seen as cardiac manifestations of sarcoidosis and may include complete heart block. In addition to conduction disorders, ventricular arrhythmias often develop, which occur in about 23% of people with heart disease. Sudden cardiac death due to ventricular arrhythmias or complete heart block is a rare complication of cardiac sarcoidosis. Cardiosarcoidosis can cause fibrosis, granuloma formation, or fluid accumulation in the heart interstitium, or a combination of the two.
Nervous system
The disease can affect any part of the nervous system. Sarcoidosis, which affects the nervous system, is known as neurosarcoidosis. The cranial nerves are most commonly affected, accounting for about 5-30% of cases of neurosarcoidosis, and paralysis of the peripheral facial nerve, often bilateral, is the most common manifestation of sarcoid from the nervous system. This happens suddenly and is usually transient. Involvement of the central nervous system is present in 10-25% of cases. Other common manifestations of neurosarcoidosis include optic nerve dysfunction, palate dysfunction, optic edema, neuroendocrine changes, hearing impairment, hypothalamic and pituitary disorders, chronic meningitis, and peripheral neuropathy. Myelopathy, an injury to the spinal cord, occurs in approximately 16-43% of neurosarcoidosis cases and is often associated with a poor prognosis of the neurosarcoidosis subtypes. In turn, paralysis of the facial nerve and acute meningitis caused by sarcoidosis tend to have the most favorable prognosis. Another common finding in sarcoidosis with neurologic involvement is neuropathy of small autonomic or sensory fibers. Neuroendocrine sarcoidosis accounts for about 5-10% of cases of neurosarcoidosis and can cause diabetes insipidus, changes in the menstrual cycle and hypothalamic dysfunction. The latter can lead to changes in body temperature, mood, and prolactin levels.
Endocrine and exocrine systems
Prolactin levels are often elevated in sarcoid, and hyperprolactinemia is noted in 3-32% of cases. This often leads to amenorrhea, galactorrhea, or nonuerpeal mastitis in women. It also often results in an increase in 1,25-dihydroxy vitamin D, active metabolite vitamin D, which is normally hydrolyzed in the kidney, but in sarcoidosis patients, vitamin D hydroxylation may occur outside the kidney, specifically within the immune cells found in disease-related granulomas. 1 alpha, 25 (OH) 2D3 is the main cause of hypercalcemia in sarcoidosis and is produced in excess by sarcoid granulomas. Gamma interferon, produced by activated macrophages and lymphocytes, plays a significant role in the synthesis of 1 alpha, 25 (OH) 2D3. Hypercalciuria (excessive excretion of calcium in the urine) and hypercalcemia (high calcium in the blood) occur in<10% людей и, вероятно, происходят от повышенного производства 1,25-дигидрокси витамина D. Дисфункция щитовидной железы наблюдается у 4,2-4,6% больных.
Parotid enlargement occurs in about 5-10% of individuals. As a rule, the involvement is two-sided. The gland is most often not painful, but elastic and smooth. Dry mouth is possible; the disease rarely affects other exocrine glands. The eyes, their glands or the parotid glands are affected in 20-50% of cases.
Gastrointestinal and genitourinary systems
Symptomatic GI involvement occurs in less than 1% of individuals (excluding the liver), and the condition most commonly affects the stomach, although the small or large intestine may also be affected in a small percentage of cases. Autopsy studies have found GI involvement in less than 10% of people. These cases likely mimic Crohn's disease, a more common granulomatous disease that affects the gut. At autopsy, nearly 1-3% of people show evidence of pancreatic involvement. Symptomatic kidney damage occurs in only 0.7% of cases, although evidence of kidney involvement at autopsy was found in 22% of people, and this occurs only in cases of chronic disease. Symptomatic involvement of the kidneys manifests itself, as a rule, in the form of nephrocalcinosis, followed by granulomatous interstitial nephritis in terms of prevalence, which manifests itself in the form of a decrease in creatinine clearance and a decrease in proteinuria. Less commonly, the epididymis, prostate, ovaries, fallopian tubes, uterus or vulva may be affected, in which case itching of the vulva is possible. In 5% of cases, autopsy reveals the involvement of the testicle. In men, sarcoidosis can lead to infertility.
About 70% of people have liver granulomas, although only 20-30% of cases show abnormal liver function tests reflecting this fact. In 5-15% of individuals, hepatomegaly is found, that is, an enlarged liver. Only 5-30% of cases of liver damage are symptomatic. Typically, these changes reflect a cholestatic pattern and include elevated alkaline phosphatase levels (the most common abnormality in liver function tests in sarcoidosis), while bilirubin and aminotransferase are only slightly elevated. Jaundice is rare.
Hematological and immunological changes
Abnormal CBCs are common, accounting for more than 50% of cases, but are not diagnostic. Lymphopenia is the most common hematologic abnormality in sarcoidosis. Anemia occurs in about 20% of people with sarcoid. Leukopenia is less common and occurs in even fewer people, but is rarely serious. Thrombocytopenia and hemolytic anemia are rare. In the absence of splenomegaly, leukopenia may reflect bone marrow involvement, but the most common mechanism is redistribution of blood T cells to disease sites. Other nonspecific features include monocytosis, which occurs in most cases of sarcoid, an increase in liver enzymes or alkaline phosphatase. People with sarcoidosis often have immunological abnormalities, such as allergies to test antigens such as Candida or a purified protein product (PPD). Polyclonal hypergammaglobulinemia is also a fairly common immunological anomaly in this disease.
Swollen lymph nodes are common in sarcoidosis and occur in 15% of patients. The size of the intrathoracic nodes increases in 75-90% of people. This usually includes hilar nodes, but most often paratracheal nodes are involved. Peripheral lymphadenopathy is very common, especially with the involvement of the cervical (usually the head and neck), axillary, epitrochlear and inguinal nodes. About 75% of cases occur with microscopic involvement of the spleen, and only 5-10% of cases actually appear splenomegaly.
Bones, joints and muscles
Bone involvement in sarcoidosis was noted in 1-13% of cases. In 5-15% of cases, the disease affects bone, joint or muscle tissue.
Sarcoidosis Videos
Sarcoidosis causes
The exact cause of the disease remains unclear. The current working hypothesis is that in genetically susceptible individuals, sarcoidosis is caused by changes in the immune response following exposure to an environmental, occupational, or infectious agent. In some cases, treatment with TNF inhibitors such as etanercept may be initiated.
Genetic
The heritability of sarcoidosis varies by race, for example, about 20% of African Americans with the condition have a family member with it, while that of white Americans is about 5%. In studies of genetic predisposition, many candidate genes have been identified, but only a few have been confirmed in further studies, and reliable genetic markers remain unknown. Currently, the most interesting candidate is the BTNL2 gene. A number of HLA-DR risk alleles are also being studied. In persistent sarcoidosis, the HLA haplotype HLA-B7-DR15 cooperates with the disease, or another gene is linked between these two loci. In unstable disease, there is a strong genetic link with HLA-DR3-DQ2.
Infectious
Several infectious agents appear to be strongly associated with sarcoidosis, but none of the known associations can be considered specific enough to suggest a direct causal role. Major infectious agents involved include mycobacteria, fungi, borrelia and rickettsia. A recent meta-analysis on the role of mycobacteria in sarcoidosis found them to be present in 26.4% of cases, but the meta-analysis also revealed possible publication bias, so the results need further confirmation. Mycobacterium tuberculosis catalase peroxidase has been identified as a possible catalyst for the sarcoidosis antigen. Transmission of the disease through organ transplantation has also been reported.
Autoimmune
The association of autoimmune disorders has been observed repeatedly. The exact mechanism of this relationship is not known, but some data support the hypothesis that this is a consequence of the prevalence of Th1 lymphokines. Delayed cutaneous hypersensitivity tests were used to measure progression.
Pathophysiology
Granulomatous inflammation is characterized primarily by the accumulation of monocytes, macrophages and activated T-lymphocytes, with an increase in the production of the main inflammatory mediators, TNF, IFN-γ, IL-2, IL-8, IL-10, IL-12, IL-18, IL-23 and TGF-β, indicating a Th1-mediated immune response. Sarcoidosis has a paradoxical effect on inflammation. It is characterized by increased activation of macrophages and CD4 helper T cells, resulting in accelerated inflammation, but the immune response to antigenic stimulation such as tuberculin is suppressed. This paradoxical state of simultaneous hyper- and hypofunction suggests a state of anergy. Anergy may also be responsible for an increased risk of infections and cancer.
Regulatory T lymphocytes at the periphery of sarcoid granulomas appear to suppress IL-2 secretion, which is believed to induce anergic state by preventing antigen-specific memory responses. Schaumann's bodies found in sarcoidosis are calcium and protein inclusions inside Langhans giant cells as part of a granuloma.
Although TNF is thought to play an important role in granuloma formation (supported by the finding that in animal models of mycobacterial granuloma formation, inhibition of TNF or IFN-γ production inhibits granuloma formation), sarcoidosis can and still develop in people treated with TNF antagonists. such as etanercept. It is likely that B cells also play a role in the pathophysiology of this disease. Serum levels of soluble HLA and ACE class I antigens are higher in individuals with sarcoidosis. Likewise, the ratio of CD4 / CD8 T cells in bronchoalveolar lavage is generally higher in individuals with pulmonary sarcoid (usually> 3.5), although it may be normal or even abnormally low in some cases. ACE levels have been found to generally correlate with total granuloma load.
Sarcoidosis has also been reported as part of HIV immune reconstitution syndrome, that is, when people are treated for HIV, their immune system recovers and as a result it begins to attack the antigens of opportunistic infections captured before said recovery, and the resulting immune response causes damage to healthy tissue.
Diagnostics
The diagnosis of sarcoidosis is by exclusion, as there are no specific tests for this condition. Chest X-ray, chest CT, CT biopsy, PET, mediastinoscopy, open lung biopsy, bronchoscopy with biopsy, endobronchial ultrasound, and endoscopic ultrasound with FNC of the mediastinal lymph node can be used to rule out sarcoidosis if it presents with pulmonary symptoms. Tissue from a lymph node biopsy undergoes both flow cytometry to rule out cancer and special staining (AFB staining and Gomori methenamine silver staining) to exclude microorganisms and fungi.
Serum markers of sarcoidosis include serum amyloid A, soluble interleukin 2 receptor, lysozyme, angiotensin converting enzyme, and KL-6 glycoprotein. An angiotensin-converting enzyme in the blood is used in the monitoring of sarcoidosis. BAL fluid may show an elevated (at least 3.5-fold) ratio of CD4 / CD8 T cells, which is evidence (but not evidence) of pulmonary sarcoid. In at least one study, the ratio of induced sputum CD4 / CD8 and TNF levels correlates with the ratio in the lavage fluid.
Differential diagnosis includes metastatic disease, lymphoma, septic embolism, rheumatoid nodules, granulomatosis with polyangiitis, chickenpox, tuberculosis, and atypical infections such as mycobacterial complex, cytomegalovirus, and cryptococcus. Sarcoidosis is most often confused with neoplastic diseases such as lymphoma, or with disorders also characterized by granulomatous inflammation of mononuclear cells, such as mycobacterial and fungal diseases.
Changes on a chest x-ray are divided into four stages:
- Stage 1: hilar lymphadenopathy
- Stage 2: hilar lymphadenopathy and reticulonodular infiltrates
- Stage 3: bilateral pulmonary infiltrates
- Stage 4: Fibrocystic sarcoidosis, usually with upward retraction of the breast, cystic and bullous changes
Although people with stage 1 x-rays tend to have acute or subacute reversible disease, people with stages 2 and 3 often have chronic, progressive disease; these models do not represent sequential "stages" of sarcoidosis. Therefore, except for epidemiological purposes, this X-ray classification is mainly of historical interest.
In sarcoidosis in the white population, thoracic lymphadenopathy and erythema nodosum are the most common initial symptoms. In this population, a gastrocnemius biopsy is a useful tool in correct diagnosis. The presence of noncaseating epithelioid granulomas in gastrocnemius muscle samples is conclusive evidence of sarcoidosis, as well as other tuberculoid and fungal diseases that are rarely histologically present in this muscle.
Classification
Specialists have identified the following types of sarcoidosis:
- annular
- erythrodermic
- ichthyosiform
- hypopigmented
- Löfgren's syndrome
- lupus fever
- morpheaform
- slimy
- neurosarcoidosis
- papular
- scar sarcoidosis
- subcutaneous
- systemic
- ulcerative.
Sarcoidosis treatment
Most people (> 75%) require only symptomatic treatment with non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin. In individuals with pulmonary symptoms, unless the disorder respiratory system are not destructive, pulmonary sarcoidosis is actively monitored, usually without therapy for 2–3 months; if inflammation does not subside spontaneously, therapy is started. Corticosteroids, usually prednisone or prednisolone, have been the standard treatment for many years. In some patients, this treatment can slow down or reverse the course of the disease, but other people do not respond to steroid therapy. The use of corticosteroids for mild form the disease is controversial, since in many cases the disease goes away spontaneously. Despite their widespread use, the evidence to support the use of corticosteroids is weak at best.
Severe symptoms are usually treated with corticosteroids, although steroid-sparing agents such as azathioprine, methotrexate, mycophenolic acid, and leflunomi are often used as alternatives. Of these, methotrexate is the most widely used and studied. Methotrexate is considered first-line treatment for neurosarcoidosis, often in combination with corticosteroids. Long-term treatment with this drug is associated with liver damage in 10% of people, and therefore can be a significant problem in people with liver damage, and therefore requires regular monitoring through liver function tests. In addition, methotrexate may be associated with pulmonary toxicity (damage to the lungs), although this is rare and more likely to distort leukopenia associated with sarcoidosis. Because of these safety considerations, methotrexate is often recommended to be combined with folic acid to prevent toxicity. Azathioprine treatment can also damage the liver. Leflunomide is used as a replacement for methotrexate, possibly due to its supposedly reduced pulmonary toxicity. Mycophenolic acid has been successfully used in the vascular form of the disease, neurosarcoidosis (especially with damage to the central nervous system; minimally effective in myopathy) and pulmonary sarcoidosis.
Since granulomas are caused by clumps of cells of the immune system, in particular T cells, some success has been achieved with the help of immunosuppressants (cyclophosphamide, cladribine, chlorambucil, cyclosporine), immunomodulatory agents (pentoxifylline and thalidomide) and anti-tumor necrosis factor (eg infliximab, etanercept , golimumab and adalimumab).
 In a clinical trial, cyclosporine in combination with prednisone did not show a significant advantage over prednisone alone in people with pulmonary sarcoidosis, although there is evidence of increased toxicity due to the addition of cyclosporine to steroids, including infections, malignancies (cancer), hypertension, and renal dysfunction. Similarly, chlorambucil and cyclophosphamide are rarely used in the treatment of sarcoidosis due to their high degree toxicity, especially the potential to cause malignancy. In clinical trials, Infliximab has been used successfully to treat pulmonary sarcoidosis in several people. Etanercept, on the other hand, failed to demonstrate significant efficacy in people with vascular sarcoidosis in a couple of clinical trials. Likewise, golimumab has not been shown to be beneficial in individuals with pulmonary sarcoidosis. One clinical trial of adalimumab showed a response to treatment in about half of the subjects, which can also be seen with infliximab, but because adalimumab is better tolerated, it may be preferred over infliximab.
In a clinical trial, cyclosporine in combination with prednisone did not show a significant advantage over prednisone alone in people with pulmonary sarcoidosis, although there is evidence of increased toxicity due to the addition of cyclosporine to steroids, including infections, malignancies (cancer), hypertension, and renal dysfunction. Similarly, chlorambucil and cyclophosphamide are rarely used in the treatment of sarcoidosis due to their high degree toxicity, especially the potential to cause malignancy. In clinical trials, Infliximab has been used successfully to treat pulmonary sarcoidosis in several people. Etanercept, on the other hand, failed to demonstrate significant efficacy in people with vascular sarcoidosis in a couple of clinical trials. Likewise, golimumab has not been shown to be beneficial in individuals with pulmonary sarcoidosis. One clinical trial of adalimumab showed a response to treatment in about half of the subjects, which can also be seen with infliximab, but because adalimumab is better tolerated, it may be preferred over infliximab.
Ursodeoxycholic acid has been used successfully to treat cases with liver involvement. Thalidomide has also been successfully tested as a treatment for persistent lupus fever in a clinical trial, which may be related to its anti-TNF activity, although its efficacy against pulmonary sarcoidosis has not been observed in a clinical trial. Skin disease can be successfully treated with antimalarial agents (such as chloroquine and hydroxychloroquine) and a tetracycline antibiotic, minocycline. Antimalarial drugs have also been shown to be effective in treating sarcoidosis-induced hypercalcemia and neurosarcoidosis. However, long-term use of antimalarial drugs is limited by their ability to cause irreversible blindness and, therefore, by the need for regular ophthalmologic examination. This toxicity is generally less for hydroxychloroquine than for chloroquine, although hydroxychloroquine may interfere with glucose homeostasis.
Recently, selective phosphodiesterase 4 (PDE4) inhibitors such as apremilast (a thalidomide derivative), roflumilast and a less subtype selective PDE4 inhibitor, pentoxifylline, have been tried for the treatment of sarcoidosis. Successful results have been achieved in the treatment of cutaneous sarcoidosis with apremilast in a small open-label study. Pentoxifylline has been used successfully for the treatment of acute illness, although its use is largely limited by its gastrointestinal toxicity (mainly nausea, vomiting, diarrhea). Clinical cases have supported the efficacy of rituximab, an anti-CD20 monoclonal antibody, and in currently a clinical trial of atorvastatin as a treatment for sarcoidosis is under way. ACE inhibitors have been reported to induce remission of cutaneous sarcoidosis and improvements in pulmonary disease, including improved lung function, remodeling of the pulmonary parenchyma, and prevention of pulmonary fibrosis in one case series study. Nicotine patches have been found to have anti-inflammatory effects in sarcoidosis patients, although disease-modifying effects require further study. Antimycobacterial treatments (drugs that kill mycobacteria, tuberculosis and leprosy) have also been shown to be effective in treating chronic cutaneous sarcoidosis in one clinical study. One small study also tried quercetin for the treatment of pulmonary sarcoid with some early success.
Due to its unusual nature, the treatment of sarcoidosis of the male reproductive tract is controversial. Thus, the differential diagnosis includes testicular cancer, so some experts recommend orchiectomy even if there is evidence of sarcoidosis elsewhere. The new approach proposed biopsy of the testis, epididymis, and resection of the largest lesion.
Forecast
The disease can pass spontaneously or become chronic, with exacerbations and remissions. In some individuals, it can progress to pulmonary fibrosis and death. About half of cases clear up without treatment or can be cleared up within 12 to 36 months, and most within 5 years. In some cases, however, the disease can persist for several decades. Two-thirds of people with this condition achieve remission within 10 years of diagnosis. With cardiac involvement, the prognosis is generally less favorable, although corticosteroids appear to be effective in improving atrioventricular conduction. The prognosis tends to be less favorable for African Americans than for Whites. People with this disease have a significantly increased risk of developing cancer, in particular lung cancer, lymphoma, and other organs that affect sarcoidosis. In sarcoidosis-lymphoma syndrome, sarcoid is associated with the development of lymphoproliferative disorders such as non-Hodgkin's lymphoma. This can be attributed to the main immunological abnormalities that occur in sarcoidosis. It can also follow cancer or occur concurrently with cancer. There are reports of hairy cell leukemia, acute myeloid leukemia and acute myeloid leukemia associated with sarcoidosis.
Epidemiology
Sarcoidosis most commonly affects young adults of both sexes, although studies have reported more cases in women. The incidence is highest for those under 40 and peaks in the 20-29 age group; the second peak is observed in women over 50.
Sarcoid occurs worldwide in all races with an average incidence of 16.5 per 100,000 men and 19 per 100,000 women. The disease is most common in the Nordic countries, with the highest annual incidence (60 per 100,000) in Sweden and Iceland. In the United Kingdom, the prevalence is 16 per 100,000. In the United States, the disease is more common in people of African descent than in whites, with annual incidences of 35.5 and 10.9 per 100,000, respectively. Sarcoidosis is less common in South America, India, Spain, Canada and the Philippines. There may be a higher susceptibility to sarcoidosis in patients with celiac disease. A link has been suggested between the two disorders.
In addition, seasonal clustering is observed in individuals with sarcoidosis. In Greece, about 70% of cases are diagnosed in March and May each year, in Spain about 50% from April to June, and in Japan, the disease is mainly diagnosed in June and July.
Differences in prevalence around the world may be at least partly due to a lack of screening programs in some regions of the world, and are obscured by the presence of other granulomatous diseases such as tuberculosis, which can interfere with the diagnosis of sarcoidosis where they are common. In addition, there may be differences in the severity of the disease between individuals. of different nationalities... Some studies suggest that people of African descent may have more severe and diffuse manifestations than whites, who are more asymptomatic. Manifestations appear to vary slightly depending on race and gender. Erythema is much more common in men than women, and in whites than in other races. The Japanese are more likely to have eye and heart lesions.
Sarcoidosis is more common in some professions, such as firefighters, educators, military personnel, people who work in pesticide industries, law enforcement, and medical personnel. Within a year after the 9/11 attacks, the prevalence of sarcoidosis has quadrupled (to 86 cases per 100,000).
History
The ailment was first described in 1877 by dermatologist Jonathan Hutchinson as a condition causing a red, raised rash on the face, arms, and hands. In 1888, another dermatologist Ernest Bénier coined the term “embittered lupus”. Later, in 1892, the histology of lupus fever was determined. In 1902, a bone lesion was first described by a group of three doctors. Between 1909 and 1910 for the first time uveitis was described in sarcoidosis, and then in 1915 by Dr. Schaumann it was noted that this is a systemic condition. Lung involvement was also described in the same year. In 1937, uveoparotid fever was first described, and in 1941 - Löfgren's syndrome. In 1958, the First International Conference on Sarcoidosis was held in London, and in 1961 a similar event was held in the United States in Washington, DC. It is also called Benier-Beck disease or Benier-Beck-Schaumann disease.
Sarcoidosis in society and culture
The World Association for Sarcoidosis and Other Granulomatous Diseases (WASOG) is an organization of physicians involved in the diagnosis and treatment of this disease and related conditions. WASOG publishes the journal Sarcoidosis, Vasculitis and Diffuse Pulmonary Diseases. In addition, the Foundation for Sarcoidosis Research (FSR) is dedicated to supporting scientific research on the disease and possible methods her treatment.
There were concerns that rescuers working on the collapse of the World shopping center are at increased risk of sarcoidosis.
In 2014, a letter to the British medical journal Lancet noted that the leader of the French Revolution, Maximilian Robespierre, suffered from sarcoidosis, and it was believed that the condition caused him a noticeable deterioration during his tenure as head of the Age of Terror.
Etymology
Sarcoidosis derives from the Greek sarco for flesh, the suffix -eidos meaning type, resembles, or similar, and -sis, a common suffix meaning condition in Greek. Thus, the whole word means "a condition resembling raw flesh." The first cases of sarcoidosis recognized in Scandinavia in late XIX in. as a new pathological unit, they appeared as cutaneous nodules resembling cutaneous sarcomas, hence the original name.
Pregnancy
Sarcoidosis usually does not interfere with a successful pregnancy and childbirth; the increase in estrogen levels during this period may even have a mild positive immunomodulatory effect. In most cases, the course of the disease does not depend on pregnancy, with improvement in some cases and worsening of symptoms in very rare cases, although it should be noted that a number of immunosuppressants (such as methotrexate, cyclophosphamide, azathioprine) used for corticosteroid-resistant sarcoidosis are teratogenic.
While studying calcium processes in the human body, I once came to the conclusion that bronchial asthma, angina pectoris, arrhythmia, hypertension and many other conditions are associated with an increase in the amount of calcium in the bloodstream and in tissues (muscle cells of the bronchial tree, muscle cells of blood vessels, muscle cells of the heart ). After long thinking about the real reasons for the increase in calcium in the bloodstream, I came to the conclusion that the real reasons have two poles. The first is associated with the constant need for calcium in the intestine in modern nutrition, to maintain an alkaline environment in the intestine. The second pole is an imbalance in thoughts, emotions and desires. In what is commonly called stress, uncontrollable, unfulfilled emotions require calcium in the tissues of the organ under stress. Both realized and unrealized emotions lead to the formation of acids. A person simply does not realize his emotions often because of various fears and doubts. The desire of a person to do something leads to the formation of energy for this action. Energy is stored in ATP, cAMP (adenosine triphosphoric acid, cyclic adenosine monophosphate) and other molecules. When the stored energy is used, the residues of phosphoric acid are cleaved from these molecules, and when finally destroyed (not used), uric acid is formed. Nervous tension, which a person often feels, at the level of biochemical processes, consists in the constant formation of cAMP and its destruction with the formation of uric acid. Subsequently, uric acid is excreted from the body through the intestines and kidneys. Of course, it is not possible to detect an increase in uric acid in the blood in the laboratory. That, the amount of uric acid and other acids that can be formed in the lungs is not enough to significantly raise its level in the blood, where it is usually sought.
Calcium, magnesium, chitosan and other molecules contribute to the elimination of uric acid from the body that has entered the intestines. By lactic acid fermentation in the intestine, lactic acid is formed from carbohydrates, which it absorbs in excess modern man... This leads to a constant increased consumption of calcium and magnesium. Enzymes of bile, pancreatic secretions and intestines can function only in an alkaline environment. Therefore, with insufficient intake of ionized calcium with food, the body is forced to constantly secrete calcium into the intestinal lumen to maintain normal digestion.
Since the quality of nutrition is supplemented by an increasing number of people, but so far not all, and only the healthiest people avoid extreme stresses, calcium is necessary for everyone. In the Republic of Belarus, it is necessary for everyone only to reduce the intake of lead and radioactive strontium into the blood.
Dear doctors! You have already seen that I am resistant to harsh criticism. This material sounds like a revolutionary idea for scientific medicine. I have no colleagues who deal with sarcoidosis "tightly". I have no colleagues who would support me in practice. I have had and still have patients, not only with sarcoidosis, who support me and, in case of hypercalcemia, take calcium supplements, get better clinical picture and stabilization of blood calcium levels. Those cases when a person receives an excess of calcium or an excess of vitamin D from food can be identified by talking with the patient. I know that last years population decline in Russia is 700,000 people annually. I know that the average Russian man does not live up to retirement. I know that average duration health workers are lower than among their patients. I know doctors sometimes get sarcoidosis. I don't need anything from you. Simply, if you deem it necessary, use the knowledge. If there is a person with adequate questions, I will be glad, as I have more questions than answers. Everything related to the scientific presentation and arguments, believe me that I know that my observations do not reach reliable (otherwise, an application for Nobel Prize wrote). And yet ... Sarcoidosis Whether I am right or wrong in my reasoning, two young men diagnosed with sarcoidosis of the lungs received relief after the measures I recommended. Two are of the two who heard me. I don't know anything about the fate of the others. The first young man worked as a bricklayer at a construction site. He complained of rapid fatigue, weakness, sweating, sleep disturbances, headache, aching heart pain, palpitations. Pulmonary sarcoidosis was detected and in the analyzes for 3 months, calcium in the serum of 2.6 mmol / L, 2.7 mmol / L, 2.8 mmol / L. According to him, the patient could not lift one brick, and he was accused of simulation and was not released from work. Having associated a long-term increase in the level of calcium in the bloodstream with its deficiency in the body, I recommended first of all calcium (it was a dietary supplement for food, today it is not such an important detail), as well as other dietary supplements. After three weeks, his health improved so much that he happily began his work. Two months later, he no longer appeared at the reception, only called and reported that he was satisfied with his health. The second case is similar, but traced to the normalization of the radiographic picture in the lungs and for about 8 more years. S.V. Khidchenko "Sarcoidosis in the practice of therapists", Minsk, Belarusian State Medical University, 2011, gives the following definition of sarcoidosis: "Sarcoidosis is a chronic multisystem relatively benign granulomatous disease of unknown etiology, characterized by the accumulation of activated T-lymphocytes (CD4 +) and mononuclear phagocytes, the formation in many organs of non-secreting epithelioid cell granulomas, disruption of the normal architecture of the affected organ or organs. " The prevalence of sarcoidosis in the Republic of Belarus is 36-38 patients per 100,000 people. The overall mortality rate from sarcoidosis is 1-5%. It is known that sarcoidosis affects the lungs in 90% of cases, and can affect the lymph nodes, spleen, salivary glands, skin, bones, joints, muscles, eyes, liver, kidneys, heart, nervous system. When a relative dies, he is buried or cremated. It is exactly the same at the cellular level. When cells die, “relatives” will dispose of their remains. The fact that in sarcoidosis lesions are found in almost any organ suggests that the causative factor can be found everywhere, or the reticuloendothelial system receives a command for widespread activation. Infection can occur everywhere, lead and other xenobiotics appear. And the command for widespread activation can come when there is little calcium ..., for example, in the intestines. Although the causes of sarcoidosis are not known, there are rational symptomatic approaches to its treatment. One of the common symptoms of sarcoidosis is an increase in serum calcium levels. Considering that the human body is a dynamic system, it is not correct to expect that the level of calcium will always be higher than normal. It may be higher than the individual relative norm at the moment. Judging by the complaints that patients present long before the detection of the disease, they are in a state of hypercalcemia. “Endocrinology”, N. Lavin, 1999, p. 431: “The cause of hypercalcemia in pulmonary sarcoidosis is ectopic synthesis and secretion of 1, 25 (OH) 2D3 (vitamin D). It is synthesized, first of all, by alveolar macrophages, which are part of sarcoid granulomas. In addition, in sarcoidosis, the regulation of metabolism 1, 25 (OH) 2D3 is impaired, its synthesis is not suppressed with an increase in calcium levels and does not depend on PTH. " Bauman V.K. Biochemistry and Physiology of Vitamin D, 1989, also links sarcoidosis with hypervitaminosis D. (More precisely, we are talking about calcitriol, the active form of vitamin D produced by the body itself). Sarcoidosis is accompanied by an increase in the level of calcium in the blood, a destructive process in the bones, often occurs after pregnancy, and affects young people under 40. The peak incidence occurs at 20-29 years, amenable to treatment with glucocorticosteroid hormones, a feature of which is blocking the absorption of calcium in the intestine and increased excretion from the body. That is, the calcium link between sarcoidosis is beyond dispute. The only question is how to relate to the increase in calcium in the bloodstream and what to do? Usually "excess" calcium is expelled by hormones. And, apparently, when a person completely reaches the edge, then his thoughts and emotions are exhausted, he directs them to survival, and not to those little things that led him to illness. That is, treatment with hormones is nothing more than a headache treatment by pressing the fingers with the door. Now, let's logically trace how this disease is related to calcium? I want to note that in our conditions, especially in a pregnant and lactating woman, it is almost unrealistic that under the influence of vitamin D so much calcium was absorbed from the intestines so that it could be superfluous and lead to destruction in various organs. What conclusions can be drawn from this? - Sarcoidosis is a calcium related disease! - Perhaps macrophages "do not know" that there is actually a lot of calcium in the blood? Or they “know” it, but someone needs calcium more and it is still not enough. - Perhaps this calcium is necessary for a nonspecific immune response, calcification of foreign bodies that enter the lungs. These can be the larvae of worms, which, as a result of their development cycle, enter the lungs. - Perhaps the bones need calcium and therefore the reticuloendothelial system takes it out everywhere and in large quantities? - Perhaps this calcium in large quantities is required in the intestines to maintain acid-base balance? The entire macrophage-histiocytic system, derived from monocytes, can respond to this request. Let me remind you that osteoclasts, alveolar, pleural and peritoneal macrophages, free and fixed macrophages of the spleen, bone marrow and lymph nodes, Kupffer cells of the liver, neuroglia cells, histiocytes are formed from monocytes. connective tissue ... Knowing that all these cells have one precursor and similar functions, utilization of dead cells, it is logical to assume, and similar enzymes. That is, I believe that if osteoclasts, destroying the osteon, direct calcium into the bloodstream, then other macrophages can destroy the surrounding tissues, filling the bloodstream with calcium. Reference: The collection of monocytes, mobile macrophages, fixed tissue macrophages and some specialized endothelial cells of the bone marrow, spleen and lymph nodes that are formed from monocytes is called the reticuloendothelial system or macrophage-histiocytic system. This phagocytic system is localized in all tissues, especially in those tissue areas where large amounts of particles, toxins and other undesirable substances must be destroyed. Numerous tissue macrophages are integral components of the alveolar walls. They can phagocytose particles trapped in the alveoli. If the particles are degraded, the macrophages digest them and release the end products into the lymph. If not digested, granulomas similar to "sarcoidosis" are formed. When deciding the question of what calcium is used to fill the bloodstream, three sources can be assumed: lungs, absorption from the intestines, and mobilization from bones. If it is based on the fact that with modern nutrition, calcium is constantly insufficient. That means hypercalcemia due to increased synthesis of Vit. D, is realized at the expense of bone calcium, and not external, therefore, it is inappropriate to reduce the amount of calcium in the diet or expel it from the body with hormones, moreover, this not only does not eliminate the cause of the disease, but also aggravates it. The entry of calcium from lung tissue into the bloodstream cannot be ruled out. But knowing that there is a concept of bone sarcoidosis, it should still be assumed that the bulk of the calcium entering the bloodstream comes from the bones. Vitamin D is designed to maintain blood calcium levels. Science knows three mechanisms for increasing calcium in the blood with the participation of vitamin D: increased absorption of calcium in the intestine, leaching of calcium from the bones and blocking the excretion of calcium by the kidneys (increased reabsorption of calcium in the distal tubules of the kidneys). It should be noted that the active form of vitamin D is synthesized by the body, and not supplied in excess with food. That is, it is not advisable to add only vitamin D to prevent rickets. It is necessary to give all the ingredients for its formation, and if vitamin D is needed, then it is synthesized. The question arises: why is it synthesized in large quantities? Who needs it? One way or another, Chinese medicine sees a direct connection between the large intestine and the lungs. The lungs are at least involved in the secretion of what comes from the large intestine into the bloodstream. It can be under-oxidized molecules, it can be chemicals that humans swallow in large quantities today, it can be bacteria and larvae of worms. Therefore, restorative measures must begin with cleansing the intestines and normalizing the functions of the digestive system. "Endocrinology", N. Lavin, 1999, p. 417: "Calcitonin. This peptide, consisting of 32 amino acids, is synthesized in the parafollicular C-cells of the thyroid gland. The secretion of calcitonin increases with an increase in the concentration of calcium in the blood and is regulated by gastroenteropancreatic hormones, in particular gastrin. I would like to note that the gastrointestinal hormonal system today is a “dark forest” for science, and this “dark forest” also scares doctors. Larvae of worms and many infections can not be looked for, but herbal complexes from worms "for prevention" can be taken. Suppress viruses, bacteria, fungi and worms polyphenols, bitterness and essential oils of herbs. In sarcoidosis, a sharp increase in the intensity of free radical reactions is observed in the tissues, against the background of antioxidant depletion. The clinical picture of sarcoidosis The first symptoms of sarcoidosis are weight loss, fever, fatigue, and loss of appetite, some of which are noted with physical activity breathing problems, dry cough, lethargy and muscle weakness. SV Khidchenko, "Sarcoidosis in the practice of therapists": "The earliest and most frequent symptom of sarcoidosis is fatigue, which the patient cannot explain in any way (70 - 80% of patients). Weakness and fatigue accompany acute and progressive forms of sarcoidosis. " (In a chronic course, such a person lives in a half-asleep state until they accidentally reveal it - my note). Almost every second patient has arthralgia (joint pain), more often the ankle joints, which can sometimes swell. Joint pain can be complemented by muscle pain (30-40%), less often chest pain. " From the side of the heart, pain, palpitations, and various heart rhythm disturbances are observed. In 1/3, peripheral lymph nodes are enlarged. The spleen may enlarge and manifest itself as a functional impairment. Patients complaining of shortness of breath, dry cough, wheezing in the lungs occur only in 20% of cases, therefore, sarcoidosis is diagnosed quite often by accident on radiography of the lungs. Other pulmonary manifestations of pleural effusion, pleural thickening and calcification, and lymph node calcifications are less common. A common companion of sarcoidosis is erythema nodosum: purplish-red, dense, painful nodules that most commonly occur on the lower legs. The adjacent joints are usually inflamed and painful. Bone changes are detected in about 10% of cases. In my opinion, in the remaining 90% of cases, they are simply not detected, as in osteoporosis and other diseases occurring with the loss of calcium from the bones. Still, 25 - 39% of patients complain of pain in the joints. Multiple isolated or confluent foci of destruction with marginal sclerosis are revealed, the structure of the bone becomes coarse-rabecular. The stomach is most commonly affected; less commonly, sarcoidosis affects the esophagus, appendix, rectum, and pancreas. Rentenologically, sarcoidosis of the spine is a polymorphic picture: more often multiple lytic foci are determined, surrounded by a zone of sclerosis at several levels; a decrease in the height of the discs, marginal bone growths, deformation of the vertebral bodies, destruction of processes and arches can be detected, paravertebral soft tissue masses can be detected. The neurological manifestations of sarcoidosis in the spine are as varied as the bone changes. The appearance of facial nerve palsy in a person should be suggestive of the likelihood of sarcoidosis. An unrecognized, persistent increase in blood calcium levels can lead to nephrocalcinosis, urolithiasis and renal failure. In rare cases, kidney damage can manifest as interstitial nephritis or as a kidney tumor. Asymptomatic granulomas can occur in any organ of the female reproductive system, as well as in the mammary glands. The most common lesion is the uterus. When the disease is started or proceeds in a severe form, complications such as a decrease in respiratory function, the formation of pulmonary fibrosis, inflammatory rashes in the eyes up to blindness, skin, lymph nodes and joints, and internal organs are affected. Treatment I believe that the wait-and-see tactics of "scientific" medicine in identifying current sarcoidosis without symptoms, as well as in compensated sacroidosis, is unacceptable. In fact, "science" leaves a person without treatment, condemning him to observation. Indications for starting treatment "science" sees when there is an increase in symptoms, the heart is involved in the process (rhythm and conduction disturbances appear), eye damage, neurological disorders. The main treatment for sarcoidosis is the administration of glucocorticosteroid hormones, which in itself reasonable person should be shocking, as the complications of such treatment themselves may be more severe than sarcoidosis. Among them, increased calcium loss leading to osteoporosis, obesity, decreased immunity, hormonal disorders, muscle weakness, arterial hypertension, mental disorders, steroid diabetes mellitus, steroid stomach and intestinal ulcers, seizures, thromboembolism, excessive hair growth in women and many others complications that are less common. It is because of this circumstance that sarcoidosis is not in a hurry to treat. But in life it turns out: “what we fought for and ran into it”. Leaving the patient under supervision, hoping for the beloved "Perhaps", without any measures, this means bringing closer the appointment of glucocorticosteroid hormones.
To normalize the alkaline state of the intestine, it is necessary to take dietary supplements with well-absorbed calcium. Since uric acid and many xenobiotics, including lead, bind chitosan, it is advisable to add chitosan in the form of Active Fiber.
Larvae of worms and many infections can not be looked for, but herbal complexes from worms "for prevention" can be taken. Suppress viruses, bacteria, fungi and worms polyphenols, bitterness and essential oils of herbs.
Improve immunity with a balanced diet with a sufficient amount of vitamins, trace elements, other antioxidants and other biologically active substances, such as adaptogens.
In sarcoidosis, a sharp increase in the intensity of free radical reactions is observed in the tissues, against the background of antioxidant depletion. Therefore, I recommend the antioxidant complexes Novomin, Sources of Purity, Elemvital with Organic Zinc, Elemvital with Organic Selenium, VitaGermaniy of the Siberian Health Corporation.