Prosthetics after complete resection of the lower jaw.
Prosthetics after complete resection of the lower jaw (according to I.M.Oksman).
The replacement prosthesis is made with sublingual protrusions for better fixation, hook loops, spring sleeves or magnets.
After resection of the jaw, the wound is sutured, a splint made of aluminum wire with hook hooks is applied to the teeth of the upper jaw, a resection prosthesis is inserted and held with rubber rings. After 2-3 weeks, the rings are removed and if the fixation by the formed scars is insufficient, then the intermaxillary fixation is used with the help of springs or magnets.
Acquired defects can be the result of inflammatory processes (osteomyelitis), specific infection (syphilis, tuberculosis), necrosis of the palate due to the erroneous administration of a solution with the properties of a protoplasmic poison (alcohol, formalin, hydrogen peroxide, etc.), surgical intervention for malignant or benign tumors, previously performed uranostaphyloplasty, as well as injuries: gunshot, household, sports. A defect of the hard palate can also occur due to its irritation with a suction prosthesis, which causes the appearance of a hematoma, followed by inflammation of the mucous membrane, periosteum and bone with its sequestration.
Significant functional disorders occur - distortion of speech, changes in breathing; frequent inflammation of the mucous membrane (rhinitis), significantly impaired swallowing, various mental disorders.
Acquired defects differ from congenital ones not only in origin, but also in that they do not have strict localization, any specific outlines; they depend on the geometric shape of the wounding projectile; along the edge of the defect, various scars are observed. On the upper jaw, there are resection of the alveolar process, unilateral and bilateral resection of the upper jaw body.
Classification of palate defects arising after gunshot wounds, inflammatory diseases and oncological operations, E.A. Kolesnikova.
By localization- defects of the anterior, posterior part and the area of the border of the hard and soft palate; one and two-sided.
According to the state of the alveolar process and the localization of the defect in it:
1) without defect of the alveolar process;
2) with a defect of the appendix (through or non-through);
3) with a defect of the process in the anterior section;
4) with a defect of the process in the lateral section.
Depending on the preservation of the abutment teeth on the upper jaw:
1) defects in the presence of teeth (on one side; on both sides; in different departments, 1-2 teeth);
2) defects in the complete absence of teeth.
According to the condition of the surrounding tissues:
1) without cicatricial changes in soft tissues near the defect;
2) with cicatricial changes (the mucous membrane of the palate, with defects in the soft tissues of the perioral region).
By defect size:
1) small (up to 1 cm);
2) medium (from 1 to 2 cm);
3) large (from 2 cm or more).
By form:
1) oval;
2) rounded;
3) undefined defects.
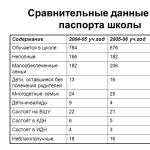
Classification of acquired defects of the upper jaw (according to L.V. Gorbaneva, with additions by B.K. Kostur and V.A. Minyaeva). According to this classification, the acquired defects of the upper jaw are divided into 7 classes:
1.defects of the alveolar part without penetration into the maxillary sinus;
2. defects of the alveolar part with penetration into the maxillary sinus;
3. defects of the bony palate: anterior, middle, lateral sections, not overlapping the alveolar part of the jaw;
4.defects of the bony palate with the capture of the lateral alveolar part
the jaw on one side, with the capture of the alveolar part from both sides, with the capture of the anterior part of the jaw;
5. defects of the bony palate and soft or only soft palate;
6. a defect formed after resection of the right or left upper jaw;
7. defect formed after resection of both upper jaws.
The defect class determines the type of prosthetics.
In the presence of acquired defects of the upper jaw and defects of the dentition without disturbing the sealing of the oral cavity (1st class), replacement dentoalveolar prostheses are made. If the defect in the upper jaw and the defect in the dentition penetrates into the maxillary sinus or nasal cavity (2nd and 4th classes of defects), then the replacement prosthesis also plays the role of an obstructing apparatus, separating the oral cavity from the maxillary sinus or nasal cavity. In cases where there are no defects in the dentition, but there are only defects of the upper jaw (3rd and 5th grade), prosthetic obturators are made to separate the oral cavity from the nasal cavity and maxillary sinus. Prostheses made in connection with the resection of the upper jaw (one or both) - the 6th and 7th class of defects are called resection prostheses.
The general principles of creating direct prostheses after resection of various parts of the jaws according to the method of I.M.Oksman are as follows:
1) semi-hot plaster models of the jaws;
2) the creation of supporting elements, which are used as crowns. If the patient is supposed to undergo radiation therapy, metal crowns are not used during the course;
3) after checking the crowns in the oral cavity, an impression is taken together with the crowns, according to which a plaster model of the jaw is obtained. Crowns are transferred to it;
4) the creation of a fixing prosthesis with clasps on the abutment teeth. The basic rule is to splinter the remaining teeth, even with a healthy periodontium. With this in mind, clasps are prepared. Modeling the fixing part from wax and replacing it with plastic;
5) half-life of the main impression from the jaw, on which the previously checked fixation plate is located. An auxiliary impression is obtained from the opposite jaw;
6) semi-hot plaster models of the jaws and plastering them into the ar-tic of the lator;
7) creation of a resection prosthesis. On a plaster model of the jaw, teeth, alveolar parts and other parts of the jaw are removed according to the plan outlined by the surgeon (phantom resection). The phantom resection line should run 4–5 mm before reaching the osteotomy line specified by the surgeon. This is necessary so that there is a space between the prosthesis and the bone wound, which provides for epithelialization of the wound, the introduction of tampons and space for granulation tissue. The surface of the fixing plate is roughened, the resulting defect is filled with wax, the base is modeled, artificial teeth are installed, plaster of paris in a cuvette and the wax is replaced with plastic.
Direct prosthetics during resection of various parts of the jaws has its own characteristics. So, with unilateral resection of the upper jaw, the artificial gum of molars and premolars is modeled with a roller extending in the anteroposterior direction. In the postoperative period, the roller forms a bed in the buccal mucosa, which will serve as an anatomical retention point.
For resection of the chin of the lower jaw
to prevent the displacement of fragments in the postoperative period, if bone grafting is delayed for a while, direct prosthetics are performed and a Vankevig splint or Rudko, Pangokhi extra-oral devices are used.
The sequence of basic manipulations when creating the device is as follows:
1) semi-hot plaster model of the lower jaw;
2) the creation of a fixing prosthesis. It is modeled from wax in the form of two removable bases (right and left) with clasps (which are prepared on the abutment teeth according to the generally accepted method). The wax is replaced with plastic;
3) after checking them in the oral cavity, the enemy takes an impression from the lower jaw, but already with fixing plates in the oral cavity, as well as an auxiliary impression from the upper jaw. The technician receives the models and casts them into the articulator in the center ratio;
4) creation of a resection prosthesis:
a) according to the plan outlined by the surgeon, teeth with a significant part of the alveolar ridge and the chin region of the jaw body are cut from the plaster model. The phantom resection is inferior in volume to the actual one. The defect is filled with wax and artificial teeth are installed. The block of artificial incisors, sometimes including the canines, is made removable so that in the postoperative period it is possible to stretch the tongue to avoid asphyxiation.
The anterior part of the prosthesis is modeled with a small chin ridge to form the soft tissues of the lower lip and chin. The chin protrusion is made collapsible, it is polymerized separately and only after the removal of the seams is attached to the prosthesis using fast-hardening plastic;
b) when resecting half of the lower jaw while preserving its branches, it is possible to displace the healthy half of the lower jaw towards the defect. To avoid this, when modeling the fixing part of the prosthesis, a removable or non-removable inclined plane adjacent to the buccal surface of the upper lateral teeth;
c) for resection of half of the lower jaw with disarticulation, the direct jaw prosthesis is made of two parts - fixing and resection.
♦ Exarticulation (lat. Ex - from, from and articulus - joint, articulation) - isolation, operation to remove the peripheral part of the limb along the line of the joint space.
The fixing part is created with multi-lamellar fixation, while adding an inclined plane, which can be removable and non-removable. It keeps the jaw fragment from displacement and is located on the vestibular side of the teeth on the healthy part of the jaw. In the absence of lateral teeth on the upper jaw, when an inclined plane cannot be used, the artificial branch is hingedly connected to the resection part of the prosthesis and made from a hollow tube for the outflow of exudate;
d) prosthetics of patients after removal of the entire lower jaw presents very great difficulties, since the prosthesis, having no bone support, is of little use for chewing solid food. Therefore, the main task of treatment is reduced to the restoration of facial contours and speech function, and in case of soft tissue defects and plastic surgery - to the formation of a skin flap. A feature of the direct prosthesis is the modeling of the basis. The inner surface of the prosthesis is rounded, but on the lingual side in the area of the lateral teeth, it should have a concavity with sublingual protrusions (this helps to keep the prosthesis in the oral cavity. In the first time after the operation, the prosthesis is fixed with hook loops to the teeth of the upper jaw, and later -
Foshar springs are used. To prevent infringement of the mucous membrane of the cheek in the prosthesis, a bed is made for the spring, and it is placed in a protective cover;
e) the obturating part of the prosthesis during the resection of half of the upper jaw is prepared as follows. After grinding a thin layer of plastic from the palatal surface of the prosthesis, the doctor applies a silicone impression mass on it and takes an impression from the operating field, using the prosthesis as an impression tray. You can get a double impression. Then, in the laboratory, the silicone mass is replaced with plastic.
For unilateral resection of the upper jaw
With unilateral resection of the upper jaw, an important role is played by the support and fixation of the resection prosthesis. Most often, the prosthesis has a one-sided bone support. On the remaining half of the upper jaw essential elements to create support are teeth, alveolar bone, hard palate. Even if the periodontal abutment teeth are healthy, they should be pre-splinted with non-removable structures.
To improve the fixation of the prosthesis, the number of clasps and occlusal patches is increased. The contact area of the occlusal pads with the teeth should be widened to minimize the displacement of the prosthesis and the overload of the abutment teeth. Retaining clasps should be positioned so as to minimize the displacement of the prosthesis and overloading of the abutment teeth: one of them is placed as close as possible to the defect, the other, possibly further, and at least one (preferably several) should be located in the interval between them.
To reduce overturning, it is advisable to use a semi-movable connection of the clasps with the base of the prosthesis. E. Ya. Vares proposed a dentoalveolar clasp for this purpose.
It is based on a pelot located on the buccal surface of the preserved teeth. The width of the pad is from the transitional fold to the equator of the teeth, the length is from the canine to the last lateral tooth, the thickness does not exceed 2.5 mm. In the distal part, the pad is semi-labilely attached to the base using a double orthodontic wire with a diameter of 0.8 mm.
To support the prosthesis great importance has an alveolar ridge, remains of a hard palate. In order to prevent overturning of the prosthesis, a support is used inside the defect: the lower wall of the orbit, the anterior surface of the temporal bone near the temporal fossa, the nasal septum and the pterygoid plate. To reduce the displacement of the resection prosthesis in the vertical direction, it is necessary to reduce its mass, making the prosthesis hollow.
The creation of a hollow resection part of the prosthesis involves the use of one of the following techniques:
... Zbarzh's technique. A model is obtained from a double impression. On it, the places to be isolated, as well as the preserved teeth, are covered with adhesive plaster or lead foil. If the model has a complex defect relief, then the undercuts are filled with the help of a parallelometer.
An individual spoon is prepared according to the usual method. Thermomass occlusal rollers are glued onto it. The central ratio of the jaws is determined and a functional impression is obtained under chewing pressure. On the model of the upper jaw, a fixing part of the prosthesis is created in the form of a cast or plastic base with clasps. For this, a modeling of the fixing part of wax is carried out, which is replaced by plastic or metal.
After checking the baseline in the oral cavity, the doctor takes an impression along with the baseline, which is transferred to the model. If the fixing part of the prosthesis is plastic, then it is modeled simultaneously with the occluding part. On the model of the upper jaw, the base of the prosthesis is prepared from one layer of base wax. The defect of the upper jaw is lined with wax, the latter is replaced with plastic after plastering the model into a cuvette. According to the defect in the jaw, a depression is formed on the prosthesis. This recess is covered in the form of a lid with a wax strip, which is replaced with plastic. The latter is connected to the prosthesis with fast-hardening plastic;
... Oksman's technique. The palatal surface of the prosthesis is ground to a thickness of 0.5-1.0 mm, then a layer of silicone impression mass is applied to the surface of the prosthesis and an imprint of the palate surface and the edges of the operating cavity is obtained (the jaw defect is pre-filled with gauze tampons, leaving only its edges exposed). A plaster model is cast from the obtained impression.
To avoid pressure ulcers, an insulating plate is applied to the plaster model in the area of the palatine suture. Then, almost the entire base is cut out of the prosthesis, leaving its clasp part and the saddle with artificial teeth, which are again superimposed on the model, and the entire base of the prosthesis is again modeled from wax. This is followed by plastering, investment and polymerization according to the rules of restoration or reconstruction of the prosthesis. Thus, a fairly lightweight jaw prosthesis is obtained with a small occlusive part and a basis of uniform thickness;
... Vares technique. A well-heated thermoplastic mass is applied to the area of the direct prosthesis adjacent to the defect, and two napkins are placed on it and the imprint of the edges and bottom of the defect is taken. Then a silicone impression paste is applied to the mass in a thin layer and the impression is reapplied to the jaw.
The resulting model is gypsum in the cuvette in the reverse way. In the cuvette, the defect area is lined with a wax plate; both parts of the cuvette are connected and disconnected. Excess wax is removed, its surface in the area of the defect is smeared with petroleum jelly and a plate of clasp wax is applied over it. The parts of the cuvette are reattached to refine the edges of the wax.
Opening the cuvette, remove the cap obtained in this way from the clasp wax. It is replaced with plastic, resulting in a thin plastic locking cap, which is smaller in size than the defect by the amount of the base wax. The cap is placed in the cuvette in the area of the defect, a self-hardening plastic is applied to the edges, and both parts of the cuvette are connected. After connecting the cap with the base, wax is melted out of the cuvette, and the base plastic is packed and polymerized. Thus, a hollow occlusive part is obtained on a direct prosthesis.
A - side view; b - front view; c - mushroom process.
In case of fractures of the lower jaw with a defect in bone tissue, fixing extracorporeal devices by A.F. Rudko, V.P. Panchokhi and their modifications are used.
^ Fracture repair toothless bottom jaw. Orthopedic devices (bus of Porta, Guning-Porta, A.A. Limberg), proposed for the treatment of fractures of the edentulous lower jaw, do not give the desired result. They are bulky and do not provide reliable fixation of edentulous fragments with significant atrophy of the alveolar part. When treating fractures in this group of patients, preference should be given to surgical methods of treatment (wire suture, needle insertion, etc.). With well-preserved alveolar ridges, as a necessary measure, the patient's prostheses can be used in combination with a chin sling.
^ Laboratory tires. Wire bars have some disadvantages. Ligatures damage the gums, they must be constantly tightened, oral hygiene is impaired. These disadvantages are devoid of laboratory-made tires. They consist of supporting crowns and an arc of orthodontic wire with a thickness of 1.5 - 2.0 mm soldered to them. To make a tire, impressions are taken. Crowns are prepared in the laboratory. They are checked in the mouth. An impression is taken from the dentition along with the crowns, into which, after its removal, the crowns are inserted and the model is cast. The arc is bent according to the model and soldered to the crowns. The splint is checked in the mouth and reinforced with cement.
^ ORTHOPEDIC TREATMENT OF CONSEQUENCES OF JAW TRAUMA
Prosthetics for false joints of the lower jaw
Treatment of fractured jaws is not always successful. In some patients, the fragments do not grow together and remain mobile. Not-
The normal mobility of the fragments of the lower jaw, the absence of callus and the formation at the ends of the fragments of a compact plate covering the bone marrow cavities, 3-4 weeks after the fracture, indicate the formation of a pseudarthrosis.
The reasons for the formation of a false joint can be general and local. The general ones include diseases that reduce the reactivity of the body and disrupt the reparative processes in the bone (tuberculosis, hypoavitaminosis, dystrophy, vascular diseases, metabolic disorders, diseases of the endocrine glands). Local factors are: 1) untimely reduction of fragments, insufficient immobilization or early removal of the splint; 2) extensive tears of soft tissues and their introduction between fragments; 3) fractures of the jaws with a bone defect of more than 2 cm; 4) detachment of the periosteum over a large extent of the jaw; 5) traumatic osteomyelitis of the jaw.
The clinical picture in the pseudarthrosis of the lower jaw is determined by the degree of mobility of the fragments, the direction of their displacement, the position of the fragments relative to each other and the upper jaw, the number of teeth in the fragments, the state of their periodontium, the size of the bone defect, the localization of the pseudarthrosis, the presence of scars of the mucous membrane and their sensitivity.
The mobility of the fragments is determined by palpation. Sometimes the displacement of fragments is observed with movements of the lower jaw. An x-ray examination is necessary to make a diagnosis.
^ Classification of the false joints of the lower jaw. IMOksman identifies four groups of false joints according to the localization of damage, the number of teeth on fragments and the size of the bone defect:
1) both fragments have 3-4 teeth:
A) with a jaw defect up to 2 cm;
B) with a jaw defect of more than 2 cm;
2) both fragments have 1 - 2 teeth;
3) defects of the lower jaw with toothless fragments:
A) with one toothless fragment;
B) with both toothless fragments;
4) bilateral defect of the lower jaw:
A) in the presence of teeth on the middle fragment,
But in the absence of teeth on the lateral fragments;
B) in the presence of teeth on "lateral fragments and in the absence of teeth on the middle.
V.Yu. Kurlyandsky considers three groups of false joints: 1) non-fused fractures within the dentition in the presence of teeth on
Breakage; 2) non-fused fractures within the dentition in the presence of toothless fragments; 3) non-fused fractures behind the dentition.
The formation of a pseudarthrosis of the lower jaw causes serious morphological and functional disorders of the dentoalveolar system. Biting and chewing food, swallowing, speech is impaired. The patient's appearance has been changed. The function of the masticatory muscles and the temporomandibular joints is impaired. Disorders are characterized by impaired coordination in the work of the right and left groups of the masticatory muscles and joints.
Treatment of nonunited fractures of the mandible must be surgical. Bone grafting and subsequent prosthetics of the dentition are performed. Prosthetics of dentition defects without restoring the integrity of the bone is carried out only in the absence of indications for surgery or the patient's refusal to undergo surgery.
The basic principle of prosthetics for patients with a pseudarthrosis of the lower jaw is that the parts of the prosthesis located on the fragments of the jaw are movably connected and should not interfere with the displacement of the fragments. Replacement of dentition defects in patients with non-fused fractures of the lower jaw with conventional prostheses will lead to a functional overload of the supporting teeth. A removable plate prosthesis without a hinge can only be used when the fragments are displaced to midline no vertical movement.
The choice of the prosthesis design is determined by the clinical picture. The presence on the fragments of a sufficient number of teeth with a healthy parodont, insignificant mobility of the jaw fragments, their correct position allows the use of articulated bridges.
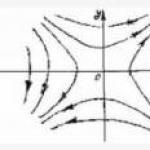
Fig. 222. Articulated prostheses for false joints of the lower jaw: a - single-joint; b - two-joint according to Oksman; c - articulated according to Gavrilov.
Not big number teeth on the jaw, a significant amplitude of displacement of fragments, a violation of the ratio of the dentition, localization of the lazh joint in the lateral part of the lower jaw is an indication for prosthetics with a schematic plate prosthesis with a hinged joint of its jaws.
Various hinges are used to connect parts of the prostheses in the false joint (I.M.Oksman, E.I. Gavrilov, V.Yu. Kurlyandsky, Z.V. Kopp, B.R. Vainshtein) (Fig. 222).
A spherical (single-joint or double-joint) joint according to Oksman provides the greatest mobility of the parts of the prosthesis. It consists of a rod with two balls at the ends. The length of the rod is 3-4 mm, the diameter is -1-2 mm and the diameter of the ball is 4-5 mm. The hinge is made from of stainless steel by casting or turning.
Gavrilov's hinge (Fig. 222c) is bent from wire. It consists of two loops connected together and located one in the vertical and the other in the horizontal planes. By changing the size of the loops, you can adjust the amplitude of movement of the parts of the prosthesis in the desired direction.
ZV Kopp proposed three types of hinges. The first type of hinge is a steel plate with two holes through which the axles are introduced. The hinge provides vertical movement of the prosthetic parts. The second type of hinge consists of a steel plate, both holes of which are connected by a slot. This allows vertical and horizontal movement. The third type of hinge consists of a rhomboid head soldered to the crown; the head is inserted into a tube reinforced in the prosthesis.
The Weinstein hinge consists of a steel coil spring inserted into sleeves that are reinforced in parts of the prosthesis. When the pseudarthrosis is localized in the area of the lower jaw angle, when one tooth is preserved on the smaller fragment, Oksman's single-joint hinge, Kopp's type III hinge and Kurlyandsky's ball-shock-absorbing clasp are used.
^ Removable hinged denture technology. Taking into account the mobility of the fragments, an impression is taken from the lower jaw with elastic impression materials without pressure with a half-open mouth. The model is used to make a removable plate prosthesis in the usual way. An auxiliary model is cast over the prosthesis. The prosthesis is sawn into two parts according to the location of the pseudarthrosis. On the lingual side, a hinge bed is created under the artificial teeth. Gavrilov's wire hinge is reinforced with quick-hardening plastic. For the Oksman hinge, grooves with a diameter of 7 mm are drilled from the lingual side of both parts of the prosthesis, departing 1 - 2 mm from the cutting line. Sleeves filled with amalgam are inserted into the recesses and a hinge is inserted.
The prosthesis is placed on the jaw and the patient uses it for 15-30 minutes. by them. As the amalgam hardens, a hinge joint forms.
With significant mobility of the fragments of the jaw or the presence of two false joints, the impression is taken from each fragment of the jaw and the basis of the prosthesis is made with clasp fixation for each fragment. After checking the basis in the oral cavity, a plaster impression is taken with them in the central occlusion. Thus, one obtains general model lower jaw.
A pseudarthrosis in case of a defect in the body of the lower jaw and a change in the position of fragments is combined with occlusion disorders. With a similar clinical picture, removable plate prostheses with hinges and a double row of teeth are used.
^ Treatment of patients with incorrectly fused jaw fractures
If, in case of damage to the jaws, specialized assistance was provided in a timely manner, the primary treatment of the wound, reposition and immobilization of fragments were correctly carried out, then the healing process proceeds favorably. The anatomical integrity of the jaw, the correct occlusion of the dentition and the function of the oral cavity are restored.
Untimely or unskilled provision of specialized care to patients with jaw fractures leads to the fusion of fragments in a vicious position, and the soft tissue wound heals with the formation of rough scars that limit the movement of the lower jaw, lips, cheeks, tongue.
With the formation of incorrectly fused fractures of the jaws, morphological and functional disorders of the dentoalveolar system are determined by the localization of the fracture, the degree of displacement of the fragments, and the severity of the deformity. The appearance of patients is changing. In case of improperly fused fractures of the upper jaw, face elongation, tension of the soft tissues of the oral region, and asymmetry of the face are observed.
Changing the position of the jaw fragments leads to speech impairment. The speech of patients suffers due to a decrease in the volume of the oral cavity and changes in the position of the articulation points. The displacement of the fragments of the lower jaw leads to a change in the position of the heads of the lower jaw in the glenoid fossa, which leads to a violation of the movement of the lower jaw, the ratio of joint elements, and dysfunction of the masticatory muscles.
The basis of functional changes is occlusive disorders. Depending on the direction of displacement of the fragments, they can be in the form of an open or cross bite. An open bite in the anterior part of the dentition is formed with Incorrectly fused fractures of the upper jaw. Lateral open bite occurs when vertically
Fecal displacements of the fragments of the lower jaw. When the fragments of the lower jaw are tilted or displaced to the midline, a cross bite is formed.
According to the degree of occlusive disorders in the horizontal plane, three groups of patients are distinguished. In the first group, occlusal contacts are preserved in the form of tubercle closure, in the second group, the teeth are closed only by the lateral surfaces, in the third group, there are no teeth closure at all.
Methods for the treatment of improperly fused jaw fractures can be surgical, prosthetic, orthodontic, and apparatus-surgical. The most expedient is surgical treatment by open (bloody) reposition of fragments and their subsequent immobilization. In case of refusal of patients from the operation or in the presence of contraindications, other methods of treatment are applied to it.
The task of orthopedic treatment includes the normalization of occlusal relationships, restoration of speech, appearance face, prevention of arthro- and myopathies. These tasks are solved by using special prostheses. Orthopedic and apparatus-surgical methods of treatment are aimed at changing the position of the teeth in the dentition and thereby creating normal occlusal contacts.
It is necessary to distinguish between two groups of patients: 1) patients with incorrectly fused fractures of the jaws and completely preserved dentition and 2) patients with incorrectly fused fractures of the jaws and partial loss of teeth.
^ Patient treatment
with improperly fused-fractures of the jaws
with fully preserved dentition
In case of improperly fused fractures of the upper jaw with the formation of an anterior open bite, the doctor's tactics depend on the degree of separation of the teeth, the patient's age and the severity of the disturbance in appearance (Fig. 223). If the interalveolar height is maintained only by the third or second molars, then contact of the anterior teeth can be achieved by grinding the molars or removing them. At a young age, orthodontic elimination of an open bite is performed according to the principles of therapy for this anomaly. With a slight gap between the front teeth, prosthetics can be made with plastic or porcelain crowns.
Lateral open bite is eliminated by prosthetics with metal-ceramic or metal-plastic aligners (Fig. 224). In young patients, positive results can be obtained by ortho-dontic restructuring of the position of the teeth.

Fig. 223 Incorrectly fused fracture of the upper jaw (observation of E N. Zhulev) "a - before treatment; b - after treatment.

Fig. 224. Treatment of an incorrectly fused fracture of the lower jaw: a - before treatment, b - after treatment with a bridge; c - a removable denture with a double row of teeth.
Crossbite with an incorrectly fused fracture of the jaw is eliminated by the orthodontic method or by prosthetics with removable dentures with a double row of teeth (Fig. 224c). The artificial teeth of a removable denture are ground to the vestibular surface of natural teeth and, thus, the occlusion is restored. In addition, to improve the appearance of patients, removable dentures have an artificial gum, which corrects the asymmetry of the face.
Prosthetics with constructions with a duplicate row of teeth has its own characteristics. First of all, difficulties arise in imposing a prosthesis on the jaw due to a change in position and alveolar parts. To solve this problem, the jaw model is studied in a parallelometer and the way of insertion of the prosthesis is determined. If the study of the model does not reveal an acceptable way of inserting the prosthesis, then the question of preparing individual teeth is decided. In difficult conditions, it is recommended to use folding or collapsible dentures. top scores gives the use of one-piece arch or prostheses with cast bases.
^ Prosthetics for patients with improperly healed fractures and partial loss of teeth
The task of prosthetics for patients in this group is to replace lost teeth with one-step restoration of the occlusion of the remaining teeth, to restore the patient's appearance and speech. Fixed or removable dentures are used depending on the number of lost teeth and on the state of their periodontium. Obtaining an impression should be attributed to the difficulties of prosthetics. It is not always possible to take an impression with a standard spoon. Therefore, a spoon is first modeled from wax in the oral cavity, and then it is replaced with plastic. The impression is taken with elastic impression materials. With the included defects of the dentition, one-piece bridges or bridges with a cast chewing surface are used. Defects in the anterior parts of the dentition are prosthetic with one-piece combined prostheses. Bridges are used to restore occlusal contacts in the vertical direction.
Crossbite due to an incorrectly fused fracture is eliminated by prosthetics with removable denture constructions. One-piece arch prostheses and removable prostheses with cast bases include occlusal onlays and artificial teeth for occlusion correction in their design. The way of insertion of removable dentures is studied in a parallelometer. Ney's clasp system allows for the fixation of the prosthesis in patients of this group.
^ Prosthetics for patients with loss of teeth with narrowing of the mouth gap (mnrostomy)
Narrowing of the oral gap (microstomy) is formed as a result of injury to the oral region, during operations for tumors, burns of the face, as well as in systemic scleroderma and tuberculous lupus.
The scars of the soft tissues surrounding the oral slit reduce their elasticity, prevent the mouth from opening and shrink the mouth. Long existing keloid scars cause deformation of the dentition and disfigure the patient's face, which in turn leads to a change in their psyche. Patients with microstomies have difficulty in contacting a doctor and often do not believe in the success of prosthetics. Narrowing of the mouth gap entails a violation of food intake and speech.
Prosthetics for patients with narrowing of the mouth gap is difficult due to the limitation of the opening of the mouth. Therefore, first of all, it is necessary to find out the possibilities of expanding the oral gap in an operative way. However, surgery is not always possible (age
Patient, general condition, systemic scleroderma, tuberculous lupus).
Prosthetics with fixed dentures for crown defects and partial loss of teeth in the lateral parts of the dentition is associated with difficulties in local anesthesia and preparation of teeth for crowns. In these cases, you can use anesthesia, premedication, etc. The separation of the lateral teeth is carried out with discs with protective heads or manually. Preparation of other surfaces of the teeth is carried out with diamond heads.
Taking an impression in patients with microstomy is also difficult due to the loss of elasticity of the soft tissues surrounding the mouth. In addition, in some patients, microstomy is combined with a defect in the alveolar ridge or with contracture of the lower jaw. This increases the volume of the impression and decreases the distance between the teeth, which makes it difficult to remove it. When prosthetics with removable dentures, the choice of the method of obtaining an impression depends on the magnitude of the narrowing of the oral gap. The impression can be obtained with a standard children's spoon or a regular standard spoon, sawn into two parts. It is best to form an individual wax spoon in the oral cavity, replace the wax with plastic and remove the impression with a hard spoon. The route of insertion and removal of the tray with the impression material is through the healthy corner of the mouth.
Difficulties in obtaining an impression with contractures of the lower jaw are associated with a lack of space between the teeth when opening the mouth. In this case, a conventional standard tray without an impression material can be introduced into the oral cavity, which cannot be done with an impression material. Therefore, the impression material should be applied to the prosthetic bed and then pressed with a spoon. After the imprint is completed, it is removed in the reverse order (first a spoon, and then an imprint).
The significant reduction in the mouth gap makes it difficult to define central occlusion in the usual way using wax templates with wax bite rolls. With a fixed interalveolar height, the central occlusion is determined with a plaster method. A roller of densely mixed plaster is introduced into the oral cavity and the patient is asked to close his teeth. Models are made from plaster prints. With a non-fixed interalveolar height, the central ratio of the jaws is determined using bite rollers and templates made of thermoplastic mass. If necessary, the rollers are already made ordinary, and the template is shortened.
The choice of a removable denture design is determined by the degree of narrowing of the oral cavity. With a significant microstomy and defects of the alveolar process, collapsible or articulated prostheses are sometimes used. However, due to the complexity of the design, they should be avoided. Prostheses should
We should be simple and accessible. Reducing the base of the prosthesis and narrowing the artificial dental arch facilitate the introduction and removal of the prosthesis from the oral cavity. When applying a removable prosthesis, the doctor must teach the patient to insert the prosthesis into the oral cavity.
^ CONTRACTURE OF THE LOWER JAW. PREVENTION AND TREATMENT
Contracture means limitation of joint mobility due to pathological changes soft tissues, bones or muscle groups functionally associated with this joint. In orthopedics and traumatology, contractures are usually divided into two main groups: a) passive (structural) and b) active (neurogenic). Passive contractures are caused by mechanical obstacles that arise both in the joint itself and in the tissues surrounding it. Passive contractures are divided into arthrogenic, myogenic, dermatogenic and desmogenic. As a separate form of contractures are distinguished ischemic, immobilization.
In patients with neurogenic contractures, neither in the area of the joint, nor in the surrounding tissues, there are no local mechanical causes that could explain the limitation of movements. Such patients usually have symptoms of loss or irritation. nervous system leading to prolonged tonic tension of individual muscle groups. Neurogenic contractures are divided into: 1) psychogenic (hysterical), 2) central (cerebral, spinal) and 3) peripheral (irritational-paretic, painful, reflex).
Most often, contracture occurs after gunshot fractures of the jaws. The presence of foreign bodies in soft tissues and bone maintains the difficulty in opening the mouth.
The unstable difficulty in opening the mouth in the first time after the injury is due to reflex contracture of the masticatory muscles, caused by pain during inflammation of the muscles and surrounding tissues. Contractures can be persistent. Most often they occur with fractures of the lower jaw in the area of its corner with damage to the masticatory muscles. Persistent restriction of mouth opening accompanies the healing of fractures of the branches of the lower jaw, condylar and coronoid processes, zygomatic arch. The cause of the contracture may be damage to the joint (arthrogenic contracture). These contractures often end in complete immobility (ankylosis) of the temporomandibular joint.
The wrong actions of the doctor can lead to the development of contracture. These include: improper primary wound care, prolonged intermaxillary immobilization, and late use of physical therapy.
To prevent the development of persistent contracture, early movements of the lower jaw are recommended. In case of fractures of the lower jaw, when the fixation of the fragments is carried out by the apparatus, therapeutic exercises are prescribed. If intermaxillary traction is used, remedial gymnastics consists of exercises for the facial muscles. A.A. Sokolov recommends the following sets of special exercises for the prevention and treatment of contractures.
^ In the first period treatment, the patient performs exercises while sitting, while the teeth are tightly clenched, and breathing is arbitrary. The first exercise is hands on the belt, slowly tilt your head back to failure, then slowly tilt it forward, trying to touch your chin to your chest. The exercise is repeated 3-4 times. The second exercise is hands on the belt, clenching your teeth, puff out your cheeks and then relax them without unclenching your teeth. Repeat the exercise 3-4 times. The third exercise is hands on the belt, turn your head to the right and left with an inclination forward, trying to touch the chest with your chin. Repeat the exercise 3-4 times in each direction. The fourth exercise is pull the tongue to the throat and then touch the tongue of the front teeth. Repeat the exercise 8-10 times. The fifth exercise is at a slow pace, tilt your head to the right and left, trying to touch the shoulder with your ear, while the shoulder rises towards the movement of the head. Repeat the exercise 2-3 times in each direction. The sixth exercise - hands on knees, close both eyes at the same time, repeating the exercise 3 times. Close one eye at a time. The seventh exercise - hands on your knees, raise and lower your eyebrows (frown). Repeat the exercise 8-10 times. The eighth exercise - hands on your knees, with the effort of facial muscles, shift the tissues of the face to the left and right. Repeat the exercise 4 - 5 times in each direction. The ninth exercise - hands on your knees, stretch your lips forward, folding them with a tube, and then stretch them, exposing your teeth. Repeat the exercise 6-8 times. Tenth exercise - hands on your knees, raise your upper lip and wrinkle your nose, followed by relaxation of the muscles involved in the movement. Repeat the exercise 6-7 times.
^ In the second period treatment after the removal of the intermaxillary traction and in the presence of a removable splint removed for the duration of the exercise, the complex of therapeutic exercises has the goal of preparing the muscles involved in the movement of the lower jaw for work. All exercises are done at a slow pace in a sitting position, hands on the belt. The duration of the lessons is 10-12 minutes.
^ First exercise. Tilting your head forward, turn your face to the right and look up over your shoulder, unclench your teeth. Return to the starting position and, after a pause of 2 - 3 seconds, repeat the exercise in the other direction. Repeat the exercise 2-3 times in each direction. Second exercise. By clenching and unclenching teeth, cut and relax
Chewing muscles. Repeat the exercise 6 times. ^ Third exercise. Holding a sheet of paper in front of you, blow on it. The duration of the exercise is 1 minute. Fourth exercise. Slowly tilting your head back and opening your mouth, try to lower the lower jaw as much as possible downward, and then turn it to its original position and, after a pause of 2 - 3 seconds, repeat the exercise 4-5 times. Fifth exercise. Opening your mouth, move the lower jaw to the right and to the left 4 - 5 times in each direction. Sixth exercise. Make vowel sounds involving lips. Repeat each sound 2-3 times. Seventh exercise. Opening your mouth, draw in your lips, unclenching your jaws, at the next moment, stretch your lips forward, squeezing your jaws. Eighth exercise. Opening your mouth, push the lower jaw forward, then return it to its original position. Repeat the exercise 8-10 times.
^ In the third period treatment after removal of immobilization, gymnastics consists of active and active-passive exercises. All exercises are done at an average pace, in a sitting position, for 18-20 minutes.
^ First exercise. Turning the head to the right and left. Repeat the exercise 6-8 times. Second exercise. Tilt your head back (inhale) return to the starting position (exhale), reaching your chin to your chest. Repeat the exercise 5 times. Third exercise. Active opening and closing of the mouth. Repeat the exercise 10-12 times. Fourth exercise. Opening your mouth, move the lower jaw to the right and to the left 10 times in each direction. Fifth exercise. Tilting your head back, open your mouth, return to the starting position and grit your teeth. Repeat the exercise 4-6 times. Sixth exercise. Tilt your head to the right and left 5 times in each direction. Seventh exercise. Turn your head to the right and tilt it back, opening your mouth. Repeat the exercise 6 times in each direction. Eighth exercise. Inflate and relax your cheeks. Repeat the exercise 10 times. Ninth exercise. Inflate the left and right cheeks alternately. Tenth Exercise. Pull your lips forward with a tube. Do the exercise 10 times. Eleventh exercise. Opening your mouth, reach your chin to your chest. Do the exercise 6 times. Twelfth exercise. Pull in your cheeks, opening your mouth, then relax your cheeks. Do the exercise 10 times. Thirteenth exercise. Perform various contractions of facial muscles within 1 minute.
The simplest means of mechanical opening of the mouth are plugs, wooden or rubber wedges, cones with a screw thread, which are inserted between the teeth for 2 - 3 hours. However, these remedies are harsh and can damage the periodontium of individual teeth. The best results are achieved with the help of devices based on the principle of active and passive jaw movements caused by elastic traction or springy processes. Currently, there are a large number of devices used in contracting
Turah and ankylosis of the jaws (Fig. 225). Mechanotherapy should be carried out after physiotherapeutic procedures (mud therapy, hydrotherapy] electrophoresis, paraffin therapy, ultraviolet irradiation). *
^ PROSTHETICS AFTER JAW RESECTION
Jaw resection is carried out for various neoplasms, and is carried out mainly by a prosthetic method. The tasks for the rehabilitation of patients with dentoalveolar defects are to restore the appearance, speech, swallowing and chewing. In addition, important for *

Fig. 225. Apparatus for mechanotherapy for jaw contraction:
A - Limberg; b - Oxman; c, d - Petrosov.
The dacha is the preservation of the remaining teeth and the prevention of atrophy of the tissues of the prosthetic bed. The solution to these problems depends on the size and topography of the acquired defect, as well as on the state of the preserved teeth and tissues of the prosthetic bed. Close cooperation of the orthopedic dentist with the surgeon makes it possible to minimize the size of the future defect and facilitate subsequent prosthetics.
Orthopedic treatment of patients after jaw resection should be staged. The stage of treatment consists in carrying out direct and distant prosthetics.
Direct prosthetics pursues following goals: 1) the formation of the future prosthetic bed; 2) prevention of scarring; 3) fixation of fragments of the lower jaw; 4) prevention of speech and chewing disorders; 5) prevention of severe deformations of the face and changes in appearance; 6) the creation of a medical and protective regime.
Direct prosthetics are not performed when resecting the lower jaw with simultaneous bone grafting. Remote prosthetics is performed after the final formation of the prosthetic bed (after 3-4 months).
The tasks of orthopedic treatment, the choice of the design of the prosthesis and the features of the prosthetics are determined by the scope of the surgical intervention. In the upper jaw, one should distinguish between resection of the alveolar process, unilateral and bilateral resection of the upper jaw body. On the lower jaw, there are resection of the alveolar part, resection of the chin of the lower jaw with loss of bone continuity, economical resection of the lower jaw while maintaining the continuity of its body, resection of half of the jaw and its complete removal.
^ Prosthetics after resection of the alveolar ridge of the upper jaw
Directly prosthetics is carried out with a removable plate prosthesis with a clasp fixation according to the method of I.M. Oksman. For this, impressions are taken from the upper and lower jaws. According to the model of the upper jaw, a fixing plate with clasps is made and checked in the oral cavity. An impression is taken from the upper jaw together with the fixing plate and the model is cast. The jaw model is cast into the occluder in the central occlusion position. On the model of the upper jaw, teeth and alveolar process are removed according to the plan outlined by the surgeon (phantom resection). The phantom resection line should extend 1 to 2 mm medially from the osteotomy line specified by the surgeon. This is necessary so that there is a space between the prosthesis and the bone wound, which ensures epithelialization of the wound.
The replacement part of the prosthesis is modeled from wax and the teeth are set. The wax is replaced by plastic in the usual manner. On the operating table, the prosthesis is applied to the jaw. Correction of occlusion and other corrections of the prosthesis are made only 2-3 days after the operation.
Remote prosthetics after resection of the alveolar process of the upper jaw is carried out with small saddle, arch and plate prostheses with retaining or musculoskeletal clasps. The number of the latter increases as the volume of the prosthesis increases. Telescopic crowns can be used. When checking the wax reproduction of the prosthesis, you should pay attention to the modeling of the replacement part of the prosthesis, which should be the support for the upper lip.
Alveolar ridge resection or parts (alveolectomy) are performed when removing benign tumors - epulids, odontomas, exostoses and other bone neoplasms, or when preparing the oral cavity for dental prosthetics.
In the latter case, partial resection of the alveolar ridge (part) is aimed at smoothing the protruding portions of the bone simultaneously with the removal of the roots of the teeth in order to obtain a flat surface for supporting the removable denture. In this case, the detected peri-root granulomas and cysts are removed.
On the site of the alveolar edge to be intervention, horizontal incisions of the mucous membrane and periosteum are made to the bone, 3 to 4 mm away from the gingival edge (upwards - on the upper jaw, downwards - on the lower jaw), along the outer surface, from the vestibule of the mouth and from the inside - from sides of the mouth. From the ends of the horizontal incision on the side of the mouth vestibule, two vertical incisions (or somewhat at an angle) are made upward, 1.5 - 2 cm long, forming a U-shaped or trapezoidal flap.
On the palatal side, the same incisions are made, but only 3-4 cm long.Mucoperiosteal flaps are peeled off on both sides, and the gum flap remaining along the ridge of the alveolar process (part) in the form of a strip is removed if there are no teeth to be removed in this area or their roots. In the latter case, first, the destroyed (or loose) teeth and roots are removed, and then the remnants of the mucous membrane of the gums, which are outside the formed mucoperiosteal flaps, are separated from them and removed.
The protruding edges of the alveoli are bite off with bone forceps, at the same time, the detected peri-root granulomas and cysts are removed. With a sharp grooved chisel and bone trays, the surface of the alveolar edge is smoothed and it is finally given a shape convenient for supporting the prosthesis. At the base of the external flap, for its greater displacement, the periosteum is incised with a horizontal incision, both flaps are placed in place and knotted sutures are applied (catgut, silk or nylon thread).
The flaps should fit snugly around the alveolar ridge (part), therefore, if folds are formed on the outer flap, the excess mucous membrane should be sparingly excised at the edge of this flap, avoiding flattening of the fornix of the vestibule of the mouth.
"Clinical operational
maxillofacial surgery ", N.М. Alexandrov
See also:
After unilateral resection of the upper jaw, a complex clinical picture, in which the conditions for fixing the prosthesis worsen. Therefore, the choice of its design and fixation methods depends on the number of teeth on the healthy side of the jaw and on their condition.
In the presence of stable and intact teeth on the healthy half of the jaw with the absence of one of the premolars or the first molar, the prosthesis is fixed with
Fig. 12-11. Obturators used for soft palate defects: a - Pomerantseva-Urbanskaya; b - Ilyina-Markosyan; c - Shildsky; d - palatine plate with obturating part in the complete absence of teeth
using 3-4 retaining clasps. Retaining clasps have the advantage that they do not interfere with the tight fit of the structure to the prosthetic bed. The tightness of the adhesion of the prosthesis to the mucous membrane is not disturbed by the subsequent atrophy of bone tissue.
In the case of an intact dentition on the healthy side, the fixation of the prosthesis can be improved by using a telescopic crown or a locking attachment on the first molar. If there are a small number of teeth on the healthy side of the jaw or their insufficient stability, the fixing part of the prosthesis is made as a supragingival splint. To fix the direct prosthesis after unilateral resection of the upper jaw, the central and lateral incisors of the healthy side are covered with interconnected crowns. If the shape of the natural crown of the distal molar of the healthy side cannot provide good fixation of the prosthesis, then it is also covered with a crown with a pronounced equator.
THEM. Oksman suggested using a three-stage technique for manufacturing a resection prosthesis of the upper jaw (Fig. 12-12). At the first stage, the fixing part of the prosthesis is prepared with clasps on the abutment teeth. For this
Chapter 12. Orthopedic treatment of patients with maxillofacial pathology 623
take an impression from a healthy area of the jaw. A fixation plate made in the laboratory is carefully fitted in the oral cavity and impressions are taken from the upper jaw. Models are cast. In this case, the fixing part of the prosthesis is placed on the model. Determine the central ratio of the jaws. Then proceed to the second stage - the manufacture of the resection part of the prosthesis. The models are placed in the articulator in the central occlusion position. On the model of the upper jaw, the border of the resection is marked in accordance with the plan of the operation. Then the central incisor on the side of the tumor is cut at the level of the cervix. This is necessary so that the prosthesis does not interfere with covering the bone with a mucosal flap. The rest of the teeth are cut at the level of the base of the alveolar process from the vestibular and palatal sides to the middle of the palate, i.e. to the fixation plate. The surface of the edge of the fixing plate is made rough, as when repairing a plastic prosthesis, and the resulting defect is filled with wax and artificial teeth are placed in occlusion with the teeth of the lower jaw. The artificial gum of the resection prosthesis in the area of the chewing teeth is modeled in the form of a roller going in the anteroposterior direction. In the postoperative period
The course of orthopedic treatment of patients ...
scars are formed along the roller, making out the bed. Subsequently, the structure is fixed with a roller with the soft tissues of the cheek. In this form, the prosthesis can be used after resection of the upper jaw as a temporary one. Later, as the surgical wound heals, the tampons are removed, and after the epithelialization of the wound surface, the obturating part of the prosthesis is made (third stage).