Reabsorption in the kidneys is the reabsorption of substances of various origins by the body from the urine. Such substances can be protein, glucose, water, sodium, organic as well as inorganic components. In the process of reverse absorption chemical substances and other components involved renal tubules, as well as epithelial cells. If chemicals are decomposition products and are in the body in excess, they are filtered out by epithelial cells. The suction process is activated in the proximal tubules.
There are several ways in which nutrients are absorbed by the body:
- Active - reabsorption of glucose, potassium, sodium ions, magnesium, amino acids. The transportation process runs against a concentration, electrochemical gradient.
- Passive - reabsorption of water, bicarbonate, urea. Transportation takes place along an electrochemical, osmotic and concentration gradient.
- Transport by pinocytosis - protein reabsorption.
Filtration speed as well as transport level chemical elements and nutrients directly depends on the quality of nutrition, the nature of the foods consumed, active image life, the presence of chronic diseases.
Views
The intake of nutrients is carried out through different channels. In this regard, reabsorption is subdivided into 2 types.
Proximal
In the process of proximal reabsorption, proteins, amino acids, fortified components and dextrose are transported from the primary urine. In this case, a full absorption of substances is observed. Filtration accounts for only 1/3 of the total volume of nutrients.
- Water reabsorption is a passive method, its speed and quality depend on the presence of hydrochloride and alkali in the filtration products.
- The transport of bicarbonate is carried out actively and passively... Its speed depends on the area of the internal organ through which urine is distributed. The passage of urine through the tubules is dynamic. The absorption of nutrients through the membrane is gradual. With passive transport, there is a decrease in urine volume and an increase in bicarbonate concentration.
- The process of reabsorption of dextrose, as well as amino acids, occurs with the direct participation of epithelial cells located in the brush border of the apical membrane. In this process, the hydrochloride is simultaneously formed and a reduced concentration of bicarbonate is observed.
- When glucose is released, a connection with the transporting cells occurs. If the glucose concentration is increased, then the transporting cells are under stress, as a result of which the component is not transported into the circulatory system.

In the process of proximal function, the maximum absorption of protein, as well as peptides, occurs.
Distal
It affects the final composition of urine, as well as the concentration of organic components. At this stage, the maximum absorption of alkali and passive transport of calcium, phosphate, potassium, and chloride ions take place.
Possible problems
If there is inadequate filtration or dysfunction of the filtering organs manifests itself, then this process can lead to the appearance of various pathologies and physiological disorders:
- Disorders of tubular reabsorption. An increase or decrease in the absorption of ions, water or organic substances from the lumen of the tubules. The causes of dysfunction arise from the decreased activity of the transporting components, lack of carriers and macroergs, epithelial injury.
- Violation of the process of secretion of epithelial cells. Injury of the distal tubules, damage to tissues and cells of the medulla or cortex of the kidneys. The presence of dysfunction is a provocateur of the development of renal and extrarenal syndromes.
- Renal syndromes - occur as a result of diuresis, disturbances in the rhythm of urination, changes in the color and nature of urine. Renal syndromes lead to the development of renal failure, tubulopathy, nephritis.
- Polyuria - diuresis, a decrease in the specific gravity of urine.
- Oliguria - a decrease in the volume of daily urine, an increase in the specific gravity of the fluid.
- Hormonal imbalance - the active production of the hormone aldosterone provokes an increase in sodium absorption, resulting in an accumulation of fluid in the body, which leads to the appearance of edema, a decrease in the presence of potassium.
- Pathology of the structure of epithelial cells - this process is the main cause of dysfunction in the control of urine concentration.
It is possible to establish the exact cause of the pathological condition using urine analysis.

Stories from our readers
"I was able to cure the KIDNEYS with the help of a simple remedy, which I learned about from the article of a DOCTOR-UROLOGIST with 24 years of experience Pushkar D.Yu ..."
Laboratory evaluation
In order to determine how the proximal reabsorption proceeds, it is required to designate the glucose concentration in the body, that is, its highest indicator.
- To determine the reabsorption of glucose, a sugar solution is injected into the patient intravenously, which significantly increases the percentage of glucose in the blood.
- A urinalysis is being examined. If the content of the compound is 9, 5 - 10 mmol / l, then this is the norm.
Other testing is done to determine the process of distal reabsorption:
- The patient should not drink any liquid for a certain time.
- A urine test is taken and the state of the fluid and its plasma is examined.
- After a certain period of time, vasopressin is administered to the patient.
- After that, it is allowed to drink water.
After studying the results of the body's reaction, it is allowed to diagnose diabetes insipidus or nephrogenic diabetes.
The normal performance of the urinary system contributes to the timely and regular elimination of toxic substances and decay products from the body. When the first symptoms of a violation of the normal functioning of the kidneys appear, an urgent need to consult a specialist. Untimely therapy or its complete absence can lead to the formation of serious complications, the development of chronic pathological processes.
Tired of fighting kidney disease?

Swelling of the face and legs, pain in the lower back, CONSTANT weakness and fatigue, painful urination? If you have these symptoms, then the chance of kidney disease is 95%.
If you don't give a damn about your health, then read the opinion of a urologist with 24 years of experience. In his article, he talks about capsules RENON DUO.
It is a fast-acting German kidney remedy that has been used all over the world for many years. The uniqueness of the drug lies in:
- Eliminates the cause of pain and brings the kidneys to their original state.
- German capsules eliminate pain already in the first course of use, and help to completely cure the disease.
- Absent side effects and no allergic reactions.
The main function of the kidneys is the processing and excretion of metabolic products, toxic, medicinal compounds from the body.
Normal kidney function contributes to normalization blood pressure, the process of homeostasis, the formation of the hormone erythropoietin.
As a result of the normal functioning of the renal system, urine is produced. The mechanism of urine formation consists of three interrelated stages: filtration, reabsorption, secretion. The appearance of malfunctions in the work of the organ leads to the development of undesirable consequences.
General concepts
Reabsorption is the absorption of substances of various origins from the urinary fluid by the body.
The process of reabsorption of chemical elements occurs through the renal canals with the participation of epithelial cells. They function as an absorbent. They distribute the elements that are contained in the filtration products.
Water, glucose, sodium, amino acids, and other ions are also absorbed and transported to the circulatory system. Chemical constituents, which are decay products, are in excess in the body and are filtered out by these cells.
The suction process takes place in the proximal tubules. Then the filtering mechanism chemical compounds passes into the loop of Henle, distal convoluted tubules, collecting ducts.
RK6L2Aqdzz0
Process mechanics
At the stage of reabsorption, the maximum absorption of chemical elements and ions necessary for the normal functioning of the body occurs. There are several ways to absorb organic components.
- Active. Substances are transported against an electrochemical concentration gradient: glucose, sodium, potassium, magnesium ions, amino acids.
- Passive. It is characterized by the transfer of the necessary components along the concentration, osmotic, electrochemical gradient: water, urea, bicarbonates.
- Transport by pinocytosis: protein.
The speed and level of filtration, transportation of the necessary chemical elements and components depends on the nature of the food consumed, lifestyle, chronic diseases.

Types of reabsorption
Depending on the area of the tubules through which the distribution of nutrients occurs, several types of reabsorption are distinguished:
- proximal;
- distal.

The proximal channel is distinguished by the ability of these channels to secrete, transfer amino acids, protein, dextrose, vitamins, water, sodium, calcium, chlorine ions, and trace elements from the primary urine.
- The release of water is a passive transport mechanism. The speed and quality of the process depends on the presence of hydrochloride and alkali in the filtration products.
- The movement of bicarbonate occurs by an active and passive mechanism. The rate of absorption depends on the area of the organ through which the primary urine passes. Its passage through the tubules is dynamic. The absorption of the components through the membrane takes a certain amount of time. The passive transport mechanism is characterized by a decrease in urine volume, an increase in bicarbonate concentration.
- The transport of amino acids and dextrose takes place with the participation of epithelial tissue... They are located in the brush border of the apical membrane. The absorption of these components is characterized by the simultaneous formation of the hydrochloride salt. At the same time, a low concentration of bicarbonate is observed.
- The release of glucose is characterized by maximum connection with the transporting cells. At a high concentration of glucose, the load on the transporting cells increases. As a result, glucose is not transferred to the circulatory system.
With the proximal mechanism, the maximum absorption of peptides and protein is observed.
Distal reabsorption affects the final composition, the concentration of organic components in the urinary substance. With distal absorption, active absorption of alkali is observed. Potassium, calcium ions, phosphates, chloride are passively transported.
The concentration of urine, the activation of absorption is due to the structural features of the renal system.

Possible problems
Dysfunctions of the filtering organ can lead to the development of various pathologies and disorders. The main pathologies include:
- Disorders of tubular reabsorption are characterized by an increase and decrease in the absorption of water, ions, organic components from the lumen of the tubules. Dysfunction occurs as a result of a decrease in the activity of transport enzymes, a lack of carriers, macroergs, trauma to the epithelium.
- Violations of excretion, secretion by epithelial cells of the renal tubules of potassium ions, hydrogen, metabolic products: para-amino hippuric acid, dioderast, penicillin, ammonia. Dysfunctions occur as a result of trauma to the distal tubules of the nephrons, damage to cells and tissues of the cortex and medulla of the organ. These dysfunctions lead to the development of renal, extrarenal syndromes.
- Renal syndromes are characterized by the development of diuresis, a deterioration in the rhythm of urination, a change chemical composition and the specific gravity of the urinary substance. Dysfunctions lead to the development of renal failure, nephritic syndrome, tubulopathy.
- Polyuria is characterized by an increase in urine output, a decrease in the specific gravity of urine. The causes of pathology are:
- excess fluid;
- activation of blood flow through the cortex of the kidneys;
- an increase in the hydrostatic pressure in the vessels;
- reducing the oncotic pressure of the circulatory system;
- violations of colloidal osmotic pressure;
- deterioration of tubular reabsorption of water, sodium ions.
- Oliguria. With this pathology, there is a decrease in daily urine output, an increase in the specific gravity of urinary fluid. The main reasons for the violation are:
- lack of fluid in the body. It occurs as a result of increased sweating, with diarrhea;
- spasm of the bringing arterioles of the kidneys. The main symptom of a violation is edema;
- arterial hypotension;
- blockage, traumatization of capillaries;
- activation of the process of transporting water, sodium ions in the distal tubules.
- Hormonal disruptions. The activation of the production of aldosterone helps to increase the absorption of sodium into the circulatory system. As a result, there is an accumulation of fluid, which leads to swelling, a decrease in the concentration of potassium in the body.
- Pathological changes in epithelial cells. They are the main cause of dysfunction in the control of urine concentration.
To establish the cause of the pathology, you can use laboratory urine tests.
jzchLsJlhIM
The normal functioning of the kidneys contributes to the timely elimination of decomposition products of chemical compounds, metabolism, and toxic elements from the body.
When the first signs of a violation of the normal functioning of an organ appear, it is necessary to consult a specialist. Untimely treatment or its absence can lead to the development of complications, chronic diseases.
Renal reabsorption is a partial return of fluid to the body with the beneficial substances it contains. And unnecessary substances are taken out. The total volume of outgoing urine is about 1.5 liters per day.
Features of urine excretion
During the day, the kidney processes about 180 liters of fluid, while not all of its volume is excreted in the urine.
Determination of reabsorption in the kidneys In order to understand how this process occurs, it is necessary to know the structural features of the kidney, and in particular the nephron. The nephron is one of the functional renal units in which the primary urine is directly filtered. The secretion of the substance, the renal corpuscle and the tubular system is what the nephron is made of.
The main components of the nephron:
- renal corpuscle - includes glomeruli and capsules; it is in it that the processing of blood plasma from liquid passing into urine takes place;
- The renal tubules are the filtration part of the nephron.
Kidney tubules are of two types: proximal and distal. The proximal tubule is the elongated and wide component of the nephron, where filtration from the capsule into the loop of Henle takes place. Henle's loops perform a connecting function in the proximal tubules with the distal ones.

Kidney Anatomy - Outline
The structure of an active cell in the sections of the nephron:
- glomerulus capsule (renal body);
- proximal tubule;
- Henle loops;
- remote tubule;
- significant part in the collecting ducts;
- collecting tube.
To carry out processing, tubular reabsorption uses the mechanisms of molecules that carry out direct transport.
The movement takes place through the membrane plasma. There are several types of transportation, which have their own characteristics.
Types of liquid transportation for filtration
Tubular reabsorption includes several types of transportation. But the main and irreplaceable are considered to be the active and passive species. They play an important role in water reabsorption.
Active transportation
- Active primary - in the process of movement, the energy obtained during the decay of the acid is used. Thanks to this type, there is a movement of useful microelements;
- Active secondary - given view active transport does not waste energy. Thanks to this type, there is a movement, processing of glucose and amino acids.
At the time of processing, the membrane is actively used, which affects the breakdown of protein, glucose with sodium ions. After the return to the cell, additional attachment of metal ions occurs. Glucose trapped in the intercellular fluid returns to the beds, passing through the capillaries. Glucose is processed only in the proximal region. This is due to the fact that it is there that the necessary type of transportation is located.

Where is reabsorption in the system
Passive transportation
Absorption occurs in the direction of movement of ions through the membrane. Rapid absorption of chloride ions occurs in the distal convoluted tubules. In other cases, processing takes place differently or not at all. It depends on the characteristics of the processed substance.
The main feature of water recycling is that it can be assimilated in different departments.
Approximately 45% is absorbed in the proximal tubule immediately after the absorption of ions. 30% is absorbed in the Henle loops, and at this moment the use of a rotary-flow mechanism takes place. In the convoluted tubules, about 25% can be absorbed, then water can be retained or excreted along with secondary urine. At the same time, the total volume of excreted secondary urine is only one percent of the amount of primary processed fluid.
Features of the processing of various substances
At the time of processing substances are used different kinds transportation. They differ from each other in the principle of action.
Filtration of glucose
Glucose is the main and universal source of human energy. For processing, it comes from the lumen of the tubule into the proximal cells with the help of a carrier, which necessarily contains a sodium ion. Mostly passive movement takes place. In the inner lining of the kidney, a high concentration of glucose occurs, which then moves into the interstitial tissue, after which it enters the general bloodstream.
With proper kidney function, glucose is completely processed. If there is a high concentration of blood in the blood, it can be assumed that there has been an overload of the tubular transport system. Because of this, there is a violation of the processing of glucose and its exit in the urine.

Reabsorption mechanisms
Filtration of amino acids
Absorption of amino acids occurs with the sodium content in the proximal tubules. The process involves an active-secondary type of delivery. In addition, additional types of transportation are actively involved, which are also used for the absorption of amino acids not only in the kidneys, but also in the gastrointestinal tract. The malabsorption process in the intestine is caused by a person's genetic disorder.
Protein filtration
With proper functioning of the kidneys and urinary system, the protein, getting into the filtration system, is completely absorbed due to panocytosis. Once in the cell, there is an osmotic pressure of chemicals that convert protein into amino acids. At the same time, there is a certain part of the protein that goes into the bloodstream unchanged.
During the day, 70 mg of protein is released with the final urine. Acceptable limits are set based on age. Physical exercise become the cause of overestimated indicators of protein content in urine.
Indicators of the norm
Tubular reabsorption has its own indicators of the norm, however, if they change, it can be assumed that a failure has occurred in the body. In order to assess the filtration capacity of the kidneys, it is necessary to undergo a series of diagnostic examinations. If a violation is detected, they will help to indicate the exact location of the pathological changes.
Biochemical data of blood and urine analysis are used as the main examination methods.
Thanks to them, it is possible to find out the glomerular rate of processing that takes place in the subcortex of the medulla, and to assess the indicators of tubular reabsorption. If violations are detected, the specialist makes the assumption that there have been changes in the excretory ability of the body or in the ability of absorption.

Reabsorption of water in the tubules
Indicators of the norm of glomerular velocity in a healthy person are from 90 to 140 ml / min. The change in indicators depends on the time of day: by the evening they will be much lower than during the day. This is due to human activity. In case of serious disturbances in the work of the body, the indicators change downward. And they increase in the postoperative period due to a decrease in blood volume. In the case of taking diuretic drugs, a decrease in indicators is observed.
Symptoms of deviations and remedies
The main symptoms of deviation are observed in the case of serious disorders of the urinary system. As a rule, in such a situation, there is a vivid picture of symptoms such as fever, a state of intoxication, pain in lumbar and in the area of the kidneys. All this indicates a violation of the urinary system. In order to prevent the appearance of renal failure, it is necessary to seek advice from the clinic.
A timely diagnosis will reduce the risk of developing serious abnormalities. Due to the violation of the filtration capacity, the kidneys remove useful and necessary substances from the body, thereby causing tremendous harm to it. In addition to the elimination of nutrients, there is a large concentration of decay products in the body.
text_fields
text_fields
arrow_upward
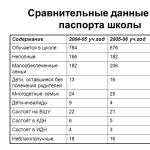
Comparison of the composition and amount of primary and final urine shows that the process of reabsorption of water and substances filtered in the glomeruli takes place in the tubules of the nephron. This process is called canal reabsorption
Depending on the department of the tubules, where it occurs, they distinguish reabsorption proximal anddistal.
Reabsorption is the transport of substances from urine to lymph and blood and depending on the mechanism of transport, passive, primary and secondary active reabsorption is isolated.
Proximal reabsorption
text_fields
text_fields
arrow_upward
Proximal reabsorption provides complete absorption of a number of primary urine substances - glucose, protein, amino acids and vitamins. In the proximal parts, 2/3 of filtered water and sodium, large amounts of potassium, divalent cations, chlorine, bicarbonate, phosphate, as well as uric acid and urea are absorbed. By the end of the proximal section, only 1/3 of the ultrafiltrate volume remains in its lumen, and, although its composition is already significantly different from blood plasma, the osmotic pressure of primary urine remains the same as in plasma.
Suction water occurs passively, along the gradient of osmotic pressure and depends on the reabsorption of sodium and chloride. Reabsorption sodium in the proximal section it is carried out by both active and passive transport. In the initial section of the tubules, this is an active process. Although sodium enters the epithelial cells through the apical membrane passively through sodium channels along a concentration and electrochemical gradient, its excretion through the basolateral membranes of epithelial cells occurs actively using sodium-potassium pumps that use ATP energy. The anion accompanying the absorbed sodium is here bicarbonate, but chlorides poorly absorbed. The volume of urine in the tubule decreases due to passive reabsorption of water, and the concentration of chlorides in its contents increases. In the terminal sections of the proximal tubules, intercellular contacts are highly permeable to chlorides (the concentration of which has increased) and they are passively absorbed from urine along a gradient. Together with them, sodium and water are passively reabsorbed. This passive transport of one ion (sodium) together with the passive transport of another (chloride) is called co-transport.
Thus, in the proximal nephron, there are two mechanisms for the absorption of water and ions:
1) active transport of sodium with passive reabsorption of bicarbonate and water,
2) passive transport of chlorides with passive reabsorption of sodium and water.
Since sodium and other electrolytes are always absorbed in the proximal tubule with an osmotically equivalent amount of water, urine in the proximal nephron remains isoosmotic to the blood plasma.
Proximal reabsorption glucose and amino acids carried out with the help of special carriers of the brush border of the apical membrane of epithelial cells. These transporters transport glucose or amino acid only if they simultaneously bind and transport sodium. Passive movement of sodium along the gradient into the cells leads to the passage through the membrane and a carrier with glucose or amino acid. To implement this process, a low concentration of sodium in the cell is required, which creates a concentration gradient between the external and intracellular environment, which is ensured by the energy-dependent operation of the sodium-potassium pump of the basement membrane. Since the transfer of glucose or amino acids is associated with sodium, and its transport is determined by the active removal of sodium from the cell, this type of transport is called reactive or symptom, those. joint passive transport of one substance (glucose) due to the active transport of another (sodium) using one carrier.
Since the reabsorption of glucose requires the binding of each of its molecules with a carrier molecule, it is obvious that with an excess of glucose, a full load of all carrier molecules can occur and glucose can no longer be absorbed into the blood. This situation is characterized by the concept "Maximum tubular tranceport of substance ", which reflects the maximum loading of tubular carriers at a certain concentration of the substance in the primary urine and, accordingly, in the blood. By gradually increasing the level of glucose in the blood and thus in the primary urine, one can easily detect the value of its concentration at which glucose appears in the final urine and when its excretion begins to linearly depend on the increase in the level in the blood. This concentration of glucose in the blood and, accordingly, in the ultrafiltrate indicates that all tubular transporters have reached the limit of their functionality and are fully loaded. At this time, glucose reabsorption is maximum and ranges from 303 mg / min in women and up to 375 mg / min in men. The value of the maximum tubular transport corresponds to the older concept "renalelimination threshold ".
Renal elimination threshold is called the concentration of a substance in the blood and in the primary urine at which it can no longer be completely reabsorbed in the tubules and appears in the final urine.
Such substances for which the elimination threshold can be found, i.e. completely reabsorbed at low concentrations in the blood, and not completely at high concentrations, are called threshold. A typical example is glucose, which is completely absorbed from the primary urine at plasma concentrations below 10 mol / L, but appears in the final urine, i.e. is not completely reabsorbed, when its content in blood plasma is above 10 mol / l. Therefore, the excretion threshold for glucose is 10 mol / L.
Substances that are not reabsorbed at all in the tubules (inulin, mannitol) or are little reabsorbed and are released in proportion to their accumulation in the blood (urea, sulfates, etc.) are called nonthreshold, since there is no elimination threshold for them.
Small amounts of filtered squirrel almost completely reabsorbed in the proximal tubules by pinocytosis. Small protein molecules are absorbed on the surface of the apical membrane of epithelial cells and are absorbed by them to form vacuoles, which, while moving, merge with lysosomes. Proteolytic enzymes of lysosomes break down the absorbed protein, after which low molecular weight fragments and amino acids are transferred into the blood through the basolateral membrane of cells.
Distal reabsorption
text_fields
text_fields
arrow_upward
Distal reabsorption of ions and water by volume is much less than proximal. However, changing significantly under the influence of regulatory influences, it determines the composition of the final urine and the ability of the kidney to excrete either concentrated or diluted urine (depending on the body's water balance). Active reabsorption occurs in the distal nephron ontria. Although only 10% of the filtered amount of cation is absorbed here, this process provides a pronounced decrease in its concentration in urine and, on the contrary, an increase in concentration in the interstitial fluid, which creates a significant osmotic pressure gradient between urine and interstitium. Chlorine absorbed mainly passively after sodium. The ability of the epithelium of the distal tubules to secrete H-ions into the urine is associated with the reabsorption of sodium ions, this type of transport in the form of exchange of sodium for a proton is called "Antiport". Actively absorbed in the distal tubule potassium, calcium and phosveils. In the collecting ducts, mainly juxtamedullary nephrons, under the influence of vasopressin, the permeability of the wall for urea and it, due to its high concentration in the lumen of the tubule, passively diffuses into the surrounding interstitial space, increasing its osmolarity. Under the influence of vasopressin, the wall of the distal convoluted tubules and collecting ducts becomes permeable to water, as a result of which it is reabsorbed along the osmotic gradient into the hyperosmolar interstitium of the medulla and further into the blood.
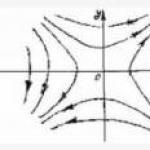
The ability of the kidney to form concentrated or diluted urine is provided by activity countercurrent multiplytubular system the kidney, which is represented by the parallel knees of the loop of Henle and the collecting ducts (Fig. 12.2).
The numbers indicate the values of the osmotic pressure of the interstitial fluid and urine. In the collecting duct, numbers in parentheses indicate the osmotic pressure of urine in the absence of vasopressin (dilution of urine), numbers without brackets indicate the osmotic pressure of urine under the action of vasopressin (concentration of urine).
Urine moves in these tubules in opposite directions (which is why the system was called countercurrent), and the processes of transport of substances in one knee of the system are enhanced ("multiplied") due to the activity of the other knee. The decisive role in the work of the countercurrent mechanism is played by the ascending knee of Henle's loop, the wall of which is impervious to water, but actively reabsorbs sodium ions into the surrounding interstitial space. As a result, the interstitial fluid becomes hyperosmotic with respect to the contents of the descending knee of the loop and towards the apex of the loop, the osmotic pressure in the surrounding tissue increases. The wall of the descending knee is permeable to water, which passively leaves the lumen into the hyperosmotic interstitium. Thus, in the descending knee, the urine becomes more and more hyperosmotic due to the absorption of water, i.e. osmotic equilibrium with the interstitial fluid is established. In the ascending knee, due to sodium absorption, urine becomes less and less osmotic and hypotonic urine ascends into the cortical part of the distal tubule. However, its amount has significantly decreased due to the absorption of water and salts in the loop of Henle.
The collecting duct, into which urine enters, also forms a countercurrent system with the ascending knee of Henle's loop. The wall of the collecting duct becomes water-permeable only in the presence of vasopressin. In this case, as urine moves through the collecting ducts deep into the medulla, in which osmotic pressure increases due to sodium absorption in the ascending knee of Henle's loop, more and more water passively goes into the hyperosmotic interstitium and urine becomes more and more concentrated.
Under the influence of vasopressin, another mechanism important for the concentration of urine is realized - the passive release of urea from the collecting ducts into the surrounding interstitium. The absorption of water in the upper parts of the collecting ducts leads to an increase in the concentration of urea in the urine, and in the lowermost parts of them, located deep in the medulla, vasopressin increases the permeability to urea and it passively diffuses into the interstitium, sharply increasing its osmotic pressure. Thus, the interstitium of the medulla becomes most highly osmotic in the region of the apex of the renal pyramids, where there is an increase in the absorption of water from the lumen of the tubules into the interstitium and the concentration of urine.
The urea of the interstitial fluid diffuses along the concentration gradient into the lumen of the thin ascending part of the loop of Henle and again enters the distal tubules and collecting ducts with the urine stream. This is how the circulation of urea is carried out in the tubules that preserve high level its concentration in the medulla. The described processes occur mainly in juxtamedullary nephrons, which have the longest Henle loops, going down deep into the medulla of the kidney.
In the medulla of the kidney there is another - vascular protivot system, formed by blood capillaries. Since the circulatory network of juxtamedullary nephrons forms long parallel straight descending and ascending capillary vessels (Fig.12.1) descending into the medulla, the blood moving along the descending straight capillary vessel gradually releases water into the surrounding interstitial space due to the increasing osmotic pressure in the tissue and, on the contrary, enriched with sodium and urea, thickens and slows down its movement. In the ascending capillary vessel, as the blood moves in the tissue with a gradually decreasing osmotic pressure, reverse processes occur - sodium and urea diffuse back into the tissue along the concentration gradient, and water is absorbed into the blood. Thus, this countercurrent system also contributes to the maintenance of high osmotic pressure in the deep layers of the tissue of the medulla, ensuring the removal of water and the retention of sodium and urea in the interstitium.
The activity of the described countercurrent systems largely depends on the speed of movement of the fluids contained in them (urine or blood). The sooner urine moves through the tubes of the countercurrent tubular system, the smaller amounts of sodium, urea and water will have time to be reabsorbed into the interstitium and large amounts of less concentrated urine will be excreted by the kidney. The higher the blood flow velocity through the direct capillary vessels of the renal medulla, the more sodium and urea the blood will carry away from the renal interstitium, because they will not have time to diffuse from the blood back into the tissue. This effect is called "Washing out" osmotically active substances from the interstitium, as a result, its osmolarity decreases, the concentration of urine decreases and more urine is excreted by the kidney low specific gravity(dilution of urine). The slower the movement of urine or blood in the medulla of the kidneys, the more osmotically active substances accumulate in the interstitium and the higher the ability of the kidney concentrate urine.
Regulation of tubular reabsorption
text_fields
text_fields
arrow_upward
Regulation of tubular reabsorption carried out as nervous, and, to a greater extent, humoral by.
Nervous influences are mainly realized by sympathetic conductors and mediators through the beta-adrenergic receptors of the membranes of the cells of the proximal and distal tubules. Sympathetic effects are manifested in the form of activation of the processes of reabsorption of glucose, sodium, water and phosphates and are realized through a system of secondary mediators (adenylate cyclase - cAMP). In the regulation of renal tissue metabolic processes, an essential role is played by the trophic influences of sympathetic nervous system... Nervous regulation of blood circulation in the medulla of the kidney increases or decreases the efficiency of the vascular countercurrent system and the concentration of urine.
The vascular effects of nervous regulation can be mediated through the intrarenal systems of humoral regulators - renin-angiotensin, kinin, prostaglandins, etc. The main factor in the regulation of reabsorption water in the distal nephron is a hormone vasopressin, formerly antidiuretic hormone. This hormone is formed in the supraoptic and paraventricular nuclei of the hypothalamus and enters the bloodstream from the neurohypophysis. The effect of vasopressin on the permeability of the tubular epithelium is due to the presence of type V-2 hormone receptors on the surface of the basolateral membrane of epithelial cells. The formation of a hormone-receptor complex (Chapter 3) entails, through the GS-protein and guanyl nucleotide, the activation of adenylate cyclase and the formation of cAMP at the basolateral membrane (Fig. 12.3).
Fig. 12.3. Mechanism of action of vasopressin on the water permeability of collecting ducts.Fig. 12.3. Mechanism of action of vasopressin on the water permeability of collecting ducts.
B-l membrane - basolateral membrane of cells,
And the membrane is the apical membrane,
GN - guanidine nucleotide, AC - adenylate cyclase.
After that, cAMP crosses the epithelial cell and, reaching the apical membrane, activates cAMP-dependent protein kinases. Under the influence of these enzymes, phosphorylation of membrane proteins occurs, leading to an increase in water permeability and an increase in the membrane surface. The rearrangement of the cell's ultrastructures leads to the formation of specialized vacuoles that carry large flows of water along the osmotic gradient from the apical to the basolateral membrane, preventing the cell itself from swelling. This transport of water through epithelial cells is realized by vasopressin in the collecting ducts. In addition, in the distal tubules, vasopressin causes the activation and release of hyaluronidases from cells, which cause the cleavage of glycosaminoglycans of the main intercellular substance and intercellular passive transport of water along the osmotic gradient.
Tubular water reabsorption
text_fields
text_fields
arrow_upward
Tubular reabsorption of water is also regulated by other hormones.
Taking into account the mechanisms of action, all hormones that regulate water reabsorption can be represented in the form of six groups:
1) increasing the permeability of the membranes of the distal nephron for water (vasopressin, prolactin, chorionic gonadotropin);
2) changing the sensitivity of cell receptors to vasopressin (parathyrin, calcitonin, calcitriol, prostaglandins, aldosterone);
3) changing the osmotic gradient of the interstitium of the medullary layer of the kidney and, accordingly, passive osmotic transport of water (parathyrin, calcitriol, thyroid hormones, insulin, vasopressin);
4) changing the active transport of sodium and chloride, and due to this, the passive transport of water (aldosterone, vasopressin, atriopeptide, progesterone, glucagon, calcitonin, prostaglandins);
5) increasing the osmotic pressure of tubular urine due to unreabsorbed osmotically active substances, such as glucose (contrainsular hormones);
6) changing the blood flow through the direct vessels of the brain substance and, thereby, the accumulation or "washing out" of osmotically active substances from the interstitium (angiotensin-II, kinins, prostaglandins, parathyrin, vasopressin, atriopeptide).
Tubular reabsorption of electrolytes
text_fields
text_fields
arrow_upward
Tubular reabsorption of electrolytes, as well as water, is regulated primarily by hormonal rather than neural influences.
Reabsorption sodium in the proximal tubules it is activated by aldosterone and is inhibited by parathyrin, in the thick part of the ascending kalen of the loop of Henle, sodium reabsorption is activated by vasopressin, glucagon, calcitonin, and is inhibited by prostaglandins E. In the distal tubule, the main regulators of sodium transport are aldosterone (activation) ...
Regulation of tubular transport calcium,phosphate and partly magnesium provided mainly by calcium-regulating hormones. Parathyrin has several sites of action in the tubular apparatus of the kidney. In the proximal tubules (straight section), calcium absorption occurs in parallel with the transport of sodium and water. The inhibition of sodium reabsorption in this section under the influence of parathyrin is accompanied by a parallel decrease in calcium reabsorption. Outside the proximal tubule, parathyrin selectively enhances calcium reabsorption, especially in the distal convoluted tubule and cortical collecting duct. Calcitriol reabsorption is also activated and suppressed by calcitonin. The absorption of phosphate in the kidney tubules is inhibited by both parathyrin (proximal reabsorption) and calcitonin (distal reabsorption), and is enhanced by calcitriol and somatotropin. Parathyrin activates magnesium reabsorption in the cortical part of the ascending knee of Henle's loop and inhibits proximal reabsorption bicarbonate.
2 stage urine formation is reabsorption - reverse absorption of water and substances dissolved in it. This has been precisely proven in direct experiments with the analysis of urine obtained by micropuncture from various parts of the nephron.
Unlike the formation of primary urine, which is the result of physicochemical filtration processes, reabsorption is largely carried out due to the biochemical processes of the cells of the nephron tubules, for which energy is drawn from the decay of macroergs. This is confirmed by the fact that after poisoning with substances blocking tissue respiration (cyanides), the reabsorption of sodium sharply deteriorates, and the blockade of phosphorylation by monoiodoacetone sharply inhibits the reabsorption of glucose. Reabsorption also worsens with a decrease in metabolism in the body. For example, when the body cools in the cold, the urine output increases.
As well as passive by transport processes (diffusion, osmosis forces), pinocytosis, electrostatic interactions between differently charged ions, etc. play an important role in reabsorption. There are also 2 types active transport:
primary active transport is carried out against an electrochemical gradient and at the same time transport occurs due to the energy of ATP,
secondary-active transport is carried out against the concentration gradient and the cell energy is not wasted. With the help of this mechanism, glucose and amino acids are reabsorbed. With this type of transport, organic matter enters the cell of the proximal tubule with the help of a carrier, which must necessarily attach a sodium ion. This complex (carrier + organic matter + sodium ion) moves in the membrane of the brush border; due to the difference in Na + concentrations between the lumen of the tubule and the cytoplasm, this complex enters the cell, i.e. there are more sodium ions in the tubule than in the cytoplasm. Inside the cell, the complex dissociates and Na + ions are removed from the cell by the Na-K pump.
Reabsorption is carried out in all parts of the nephron, with the exception of the Shumlyansky-Bowman capsule. However, the nature of reabsorption and intensity in different parts of the nephron is not the same. In the proximal parts of the nephron, reabsorption is very intensive and depends little on water-salt metabolism in the body (obligatory, obligatory). In the distal parts of the nephron, reabsorption is very variable. This is called facultative reabsorption. It is the reabsorption in the distal tubules and collecting ducts, to a greater extent than in the proximal part, that determines the function of the kidney as an organ of homeostasis, regulating the constancy of osmotic pressure, pH, isotonia and blood volume.
Reabsorption in various parts of the nephron
Reabsorption of ultrafiltrate occurs by the cuboid epithelium of the proximal tubule. Here have great importance microvilli. In this section, glucose, amino acids, proteins, vitamins, trace elements, a significant amount of Na +, Ca +, bicarbonates, phosphates, Cl -, K + and H 2 O are completely reabsorbed. In the subsequent sections of the nephrons, only ions and H 2 O are absorbed.
The mechanism of absorption of the listed substances is not the same. The most significant in terms of volume and energy consumption is Na + reabsorption. It is provided by both passive and active mechanisms and occurs in all parts of the tubules.
Active reabsorption of Na causes a passive exit from the tubules of Cl ions - which follow Na + due to electrostatic interaction: positive ions entrain negatively charged Cl - and other anions.
In the proximal tubules, about 65-70% of the water is reabsorbed. This process is carried out due to the difference in osmotic pressure - passively. The transition of water from the primary urine equalizes the osmotic pressure in the proximal tubules to the level in the tissue fluid. 60-70% of calcium and magnesium is also reabsorbed from the filtrate. Their further reabsorption continues in the loop of Henley and the distal tubules, and only about 1% of filtered calcium and 5-10% of magnesium are excreted in the urine. The reabsorption of calcium and, to a lesser extent, magnesium is regulated by parathyroid hormone. Parathyroid hormone increases the reabsorption of calcium and magnesium and reduces the reabsorption of phosphorus. Calcitonin has the opposite effect.
Thus, in the proximal convoluted tubule, all proteins, all glucose, 100% amino acids, 70-80% water, а, Сl, Mg, Ca are reabsorbed. In the loop of Henley, due to the selective permeability of its sections for sodium and water, 5% of the ultrafiltrate is additionally reabsorbed and 15% of the volume of primary urine enters the distal part of the nephron, which is actively processed in the convoluted tubules and collecting tubes. The volume of the final urine is always determined by the water and salt balance of the body and can range from 25 liters per day (17 ml / min) and up to 300 ml (0.2 ml / min).
Reabsorption in the distal nephron and collecting ducts ensures the return of an ideal osmotic and saline fluid into the blood, maintaining a constant osmotic pressure, pH, water balance and stability of ion concentration.
The content of many substances in the final urine is many times higher than in plasma and primary urine, i.e. passing through the tubules of the nephron, the primary urine is concentrated. The ratio of the concentration of a substance in the final urine to the concentration in plasma is called concentration index... This index characterizes the processes that occur in the nephron tubule system.
Reabsorption of glucose
The concentration of glucose in the ultrafiltrate is the same as in the plasma, but in the proximal nephron it is almost completely reabsorbed. Under normal conditions, no more than 130 mg is excreted in the urine per day. Reabsorption of glucose occurs against a high concentration gradient, i.e. reabsorption of glucose occurs actively, and it is transferred using the mechanism of secondary active transport. The apical membrane of the cell, i.e. the membrane facing the lumen of the tubule passes glucose only in one direction - into the cell, and does not let it back into the lumen of the tubule.
There is a special glucose transporter in the apical membrane of the proximal tubule cell, but glucose must be converted to glu-6 phosphate before interacting with the transporter. The membrane contains the enzyme glucokinase, which provides phosphorylation of glucose. Glu-6-phosphate binds to the apical membrane transporter simultaneously with sodium.
This complex due to the difference in sodium concentration ( there is more sodium in the lumen of the tubule than in the cytoplasm) moves in the membrane of the brush border and enters the cell. In the cell, this complex dissociates. The carrier returns for new portions of glucose, while glu-6-phosphate and sodium remain in the cytoplasm. Glu-6-phosphate, under the influence of the enzyme glu-6-phosphatase, breaks down into glucose and a phosphate group. The phosphate group is used to convert ADP to ATP. Glucose travels to the basement membrane, where it combines with another carrier, which transports it across the membrane into the blood. Transport across the basement membrane of the cell is of facilitated diffusion and does not require the presence of sodium.
The reabsorption of glucose depends on its concentration in the blood. Glucose is completely absorbed if its concentration in the blood does not exceed 7-9 mmol / l, normally it is from 4.4 to 6.6 mmol / l. If the glucose content is higher, then part of it is not reabsorbed and is excreted in the final urine - glucosuria is observed.
On this basis, we introduce the concept about the threshold withdrawal. Elimination threshold(the threshold of reabsorption) is the concentration of a substance in the blood at which it cannot be completely reabsorbed and enters the final urine . For glucose, this is more than 9 mmol / L, because in this case, the capacity of the carrier systems is insufficient and sugar enters the urine. In healthy people, this can be observed after the intake of large amounts of it (alimentary (food) glucosuria).
Reabsorption of amino acids
Amino acids are also completely reabsorbed by the cells of the proximal tubule. There are several specific reabsorption systems for neutral, dibasic, dicarboxylic and imino acids.
Each of these systems provides for the reabsorption of several amino acids of the same group:
1 group - glycine, proline, hydroxyproline, alanine, glutamic acid, creatine;
Group 2 - dibasic - lysine, arginine, ornithine, histidine, cystine;
Group 3 - leucine, isoleucine.
Group 4 - Imino acids - organic acids containing a divalent imino group (= NH) in the molecule, heterocyclic imino acids proline and hydroxyproline are part of proteins and are usually considered amino acids.
Within each system, there is a competitive relationship between the transfer of individual amino acids included in a given group. Therefore, when there is a lot of one amino acid in the blood, the carrier does not have time to transport all the amino acids of this series - they are excreted in the urine. Amino acids are transported in the same way as glucose, i.e. by the mechanism of secondary active transport.
Protein reabsorption
The filtrate receives 30-50 g of protein per day. Almost all protein is completely reabsorbed in the tubules of the proximal nephron, and in a healthy person there are only traces of it in the urine. Proteins, unlike other substances, are reabsorbed into cells by means of pinocytosis. (Molecules of the filtered protein are adsorbed on the surface membrane of the cell, ultimately forming a pinocytic vacuole. These vacuoles fuse with the lysosome, where proteins are cleaved under the influence of proteolytic enzymes and their fragments are transferred into the blood through the basal cytoplasmic membrane). With kidney disease, the amount of protein in the urine increases - proteinuria. It can be associated either with impaired reabsorption, or with an increase in protein filtration. May occur after physical exertion.
The metabolic products, which are harmful to the body, excreted from the body, do not undergo active reabsorption. Those compounds that are not able to penetrate the cell by diffusion do not return to the blood at all and are excreted in the urine in the most concentrated form. These are sulfates and creatinine, their concentration in the final urine is 90-100 times higher than in plasma - this is thresholdless substances. The end products of nitrogen metabolism (urea and uric acid) can diffuse into the epithelium of the tubules, therefore they are partially reabsorbed, and their concentration index is lower than that of sulfates and creatinine.
From the proximal convoluted tubule, isotonic urine enters the loop of Henle. Approximately 20-30% of the filtrate comes here. It is known that the loop of Henle, distal convoluted tubules and collecting ducts is based on the mechanism countercurrent and multiplying tubular system.
Urine moves in these tubules in opposite directions (which is why the system was called countercurrent), and the processes of transport of substances in one knee of the system are enhanced (“multiplied”) due to the activity of the other knee.
The principle of a countercurrent system is widespread in nature and technology. This is a technical term that defines the movement of two flows of liquid or gases in opposite directions, creating favorable conditions for exchange between them. For example, in the limbs of Arctic animals, arterial and venous vessels are located close, blood flows in parallel arteries and veins. Therefore, arterial blood warms the cooled venous blood moving to the heart. The contact between them turns out to be biologically beneficial.
This is how the loop of Henle and the rest of the nephron are arranged and work, and the mechanism of a countercurrent-multiplying system exists between the knees of the loop of Henle and the collecting tubes.
Let's take a look at how Henle's loop works. The descending section is located in the medulla and stretches to the apex of the renal papilla, where it bends 180 and passes into the ascending section, located parallel to the descending one. The functional significance of different sections of the loop is not the same. The descending part of the loop is well permeable to water, and the ascending one is waterproof, but actively reabsorbs sodium, which increases the osmolarity of the tissue. This leads to an even greater outflow of water from the descending part of the loop of Henle along the osmotic gradient (passively).
Isotonic urine enters the descending knee, and at the top of the loop, the concentration of urine increases 6-7 times due to the release of water, therefore, concentrated urine enters the ascending knee. Here, in the ascending knee, sodium is actively reabsorbed and chlorine is absorbed, water remains in the lumen of the tubule and hypotonic fluid (200 osmol / l) enters the distal tubule. Between the segments of the knee of the loop of Henle, there is always an osmotic gradient of 200 milliosmoles (1 osmol = 1000 milliosmoles - the amount of a substance that develops an osmotic pressure of 22.4 atm in 1 liter of water). Along the entire length of the loop, the total difference in osmotic pressure (osmotic gradient or drop) is 200 milliosmoles.
Urea also circulates in the turn-countercurrent system of the kidney and is involved in maintaining high osmolarity in the renal medulla. Urea leaves the collecting tube (when the final urine moves into the pelvis). It enters the interstitium. Then it is secreted into the ascending knee of the nephron loop. Then it enters the distal convoluted tubule (with urine flow), and again ends up in the collecting tube. Thus, the circulation in the medulla is a mechanism for maintaining the high osmotic pressure that the nephron loop creates.
In the loop of Henle, another 5% of the initial volume of the filtrate is reabsorbed, and about 15% of the volume of primary urine flows from the ascending part of the loop of Henle into the convoluted distal tubules.
An important role in maintaining high osmotic pressure in the kidney is played by the direct renal vessels, which, like the loop of Henle, form a turn-countercurrent system. Descending and ascending vessels run parallel to the nephron loop. The blood moving through the vessels, passing through layers with gradually decreasing osmolarity, gives up salt and urea to the intercellular fluid and captures water. So the countercurrent vascular system is a shunt for water, thereby creating conditions for the diffusion of solutes.
The processing of primary urine in the Henle loop ends the proximal reabsorption of urine, due to which 100-105 ml / min from 120 ml / min of primary urine returns to the blood, and 17 ml goes further.