Male infertility or the temporary inability to conceive a child due to pathology is a very common phenomenon today. According to statistics, 55% of men experience temporary difficulties in conceiving a new life, of which 15-20% cannot irrevocably have children. Today, when patients take a spermogram, doctors are more likely to observe abnormal sperm. And the pathology of the sperm head is the most common anomaly.
What are the pathological forms of sperm, the causes and treatment of the anomaly, we will tell in this article.
Sperm pathology: what happens to the reproductive cells
In medicine, there is such a term as teratozoospermia. He says that in the male body there are pathological spermatozoa with a disturbed structure and shape. This defect can be observed in the body, head, and tail of the sperm. This kind of anomaly in the spermogram indicates that the patient will not be able to have children, since deformed sperm cells, even if they fertilize an egg, the risk that a child will be born with a genetic pathology is very high.
You need to conceive children in absolute health. Very often, doctors state the deformation of the sperm head. In this state, various processes take place. The head can be either very small or larger than its standard size. Sometimes there is a sperm with two heads at the same time. In fact, a damaged sperm head leads to deformation of the entire sperm. That is why you need to start treatment as soon as possible.
Types of deformation of the sperm head
In fact, one healthy sperm can fertilize an egg, but in the natural environment there should be about 15 ml of sperm ready for fertilization in the male body. In this case, the volume of ejaculate should be 2-2.5 ml. For conception, 50 thousand spermatozoa are allowed, since during natural selection damaged, weak and inactive spermatozoa are eliminated, leaving only healthy and strong ones.
If the spermogram shows more than 50% of damaged sperm, conception is almost impossible. This condition is influenced by many factors. Deformed sperm can have the following head structure:
- Macrohead. This is when the head has a significant size in relation to the neck and tail;
- Microhead. In this case, the head, on the contrary, is small in comparison with the body of the sperm;
- Double. In this form, two heads grow from the neck. It is also possible that two necks grow from one head;
- Pear-shaped. The head is pear-shaped and somewhere even cone-shaped;
- Pathological head. In this case, the structure of the base is deformed. The head is not oval, round, but wrinkled and flattened;
- Cervical pathology. In this situation, the neck has a zigzag shape. Because of what sperm becomes inactive and lifeless.

But if in the first four cases such a head shape can also be found in a healthy man, but prevails in a smaller amount, then in the other two cases the situation indicates the presence of pathology. Why does sperm deformation occur?
Causes of Defective Sperm
A man may not even guess that his sperm is quantitatively and qualitatively far from ideal. Usually, pathological processes in the semen do not make themselves felt. The problem can open up when partners cannot conceive a child. In this case, they turn to specialized centers where they undergo examinations. The man is invited to undergo a spermogram.
This analysis is able to reveal how viable the sperm are, what shape and structure they have, it is possible to detect defective sperm.
Pathological phenomena of the sperm head can be triggered by various factors. These include:
- Hormonal imbalance. An imbalance can develop against the background of inflammatory processes, but often the production of hormones is largely influenced by stress, overwork;
- Genetic predisposition. If a man had problems with head pathology in a family, then in 95% of cases such an anomaly will develop in him;
- Age. Age-related changes also affect sperm health. Men who have had andropause (male menopause) have more damaged sperm. This occurs at the hormonal level, when the body produces less androgen and testosterone;
- Infections (viruses, bacteria). It has long been proven that diseases of the genitourinary system lead to deterioration of sperm in the seminal fluid;
- Varicocele. Specialists highlight the expansion of the veins in the scrotum as a separate item. It is this ailment that most adversely affects the structure and shape of the sperm, preventing them from developing in a natural way;
- Injuries. Any trauma in the scrotum, penis, testicles can alter sperm and lead to abnormal formation of germ cells. Blows, falls, surgery can lead to deformed sperm;
- Addictions. Alcohol and smoking negatively affect the formation of new germ cells. Nicotine destroys the protective layer of the body, alcohol slows down the production of testosterone, as a result of which abnormal sperm is formed;
- Inflammation. Usually, the connection between deformed sperm and inflammation is very thin, since with focal diseases of the scrotum and testicles, a qualitative and quantitative change occurs in the spermogram.

How to cure head pathology: medication
Of course, having this kind of problem, the patient goes to the doctor. There is no single protocol for treating abnormal sperm cells. The presented type of infertility has a different etiology. Therefore, a specialist, first of all, eliminates the origins of the disease, which leads to the normalization of sperm in the body.
With infectious diseases, the patient is prescribed antibiotic therapy. With inflammatory - anti-inflammatory. If the anomaly is caused by a hormonal imbalance, the doctor may prescribe a consultation with an andrologist and an endocrinologist. In this case, the patient is prescribed hormone therapy.
To identify the cause of infertility in men, a study is carried out, during which it is compiled, which makes it possible to isolate pathological forms of spermatozoa. Presence in ejaculate a large number sperm with an abnormal morphology, called teratozoospermia. The study of these germ cells occurs exclusively under a microscope after their immobilization, for the implementation of which various types of spermogram are used.
What are the pathological forms of sperm?It is customary to isolate the following abnormal forms of the sperm:
- cervical pathology;
- tail pathology.
With the first type of pathology, a large, less often giant sperm head is usually detected. This violation is called macrocephaly. There may also be sperm with a disproportionately small head size - microcephaly. The cause of the pathology of the sperm head can be as unfavorable factors, genetic predisposition, and hormonal disorders. In addition, this pathology often occurs after a viral infection, which leads to the development of inflammation of the testicles.
In case of pathology in the cervical region, an abnormal discharge of the flagellum is observed, the angle is usually less than 180 degrees. In case of pathology in the tail region, such forms as shortening, fracture of the flagellum, doubling, etc. are usually distinguished.
In the presence of several pathologies at once, in different parts of the sperm, they speak of the development of polyanomal spermatozoa.
What are the parameters of sperm examination?When conducting a spermogram, for making diagnoses to sick men, many parameters are taken into account.
- Ejaculate dilution time. Sperm is not liquid immediately after discharge. This usually takes 10 to 60 minutes. With an increase in this interval, or a complete absence of liquefaction, they speak of a violation in the work of the prostate gland. However, the relationship between this parameter and the presence of infertility in a man has not been identified to date.
- Semen volume. Normally, this parameter is 3-4 ml. The volume of ejaculate plays an important role in the fertilization process, because the seminal fluid itself is nothing more than foreign cells for the female body, the appearance of which leads to a suppression of the immune system.
- The number of sperm in the semen. When carrying out any type of spermogram, this parameter is the most important. The concentration of sperm in the ejaculate should be 60-120 million per 1 ml.
- Sperm motility. Normally, the spermogram shows 60-70% of active and up to 10-15% of inactive spermatozoa. The number of motionless usually does not exceed 10-15%. With pathology, this figure rises sharply. This pathology is observed in those men whose work is associated with high temperatures, for example, a cook, a bath attendant, etc.
Spermogram is a fairly informative research method. It is with the help of a spermogram that the presence of pathological forms of spermatozoa is revealed and treatment is prescribed.
The entire therapeutic process is aimed at reducing the number of abnormalities in the semen and increasing the number of motile sperm. However, in most cases, the only option for resolving this problem is IVF, before which, from the sperm taken from a man, the most mobile sperm are selected, and with the absence of abnormalities.
For the timely detection of pathology and treatment of the disease, each man, for the purpose of prevention, must undergo an examination and do a spermogram.
- Changes in the structure of the head of the reproductive cell. It can be enlarged and called a macrocephalus. However, there is also microcephaly, that is, the sperm head is very small.
- If the flagellum is attached to the head of the reproductive cell at an angle of less than 180⁰, then the pathology of the neck structure is declared.
- There are also violations in the structure of the tail section. In this case, the sperm have very small tails. They can be thickened or thinned, which is determined by the spermogram.
- Sex cells may not contain chromosomal material at all.
- The presence of vacuoles in the head of the cell is also interpreted as a pathology of the head.
2 Reasons for violations
Such violations of the structure of gametes are not spontaneous. The pathology of the head or other part of the cell can be triggered by one or more unfavorable factors that affect the man's body. What can cause anomalies?
- Malfunctions of the patient's hormonal system.
- Spermogram can be atypical as a result of genetic abnormalities.
- Chromosome abnormalities can be triggered by the advanced age of the patient.
- Often pathological spermatozoa appear after the transferred infectious diseases, including those of viral genesis.
- Constant or periodic exposure to negative production factors can also lead to the appearance of abnormal cell structure.
- Pathological inflammations of a non-infectious nature.
- Injuries to the perineum and genitals.
- Poor nutrition and bad habits.
- Head pathology can be triggered by prolonged emotional or physical stress.

3 Pathology of gametes
Before considering in which case a violation in the spermogram can lead to the impossibility of fertilization of the egg, we determine what is considered the norm. Experts believe that the presence of less than half of the abnormal spermatozoa in the ejaculate in a healthy man makes it possible for the patient to have healthy offspring. Some even admit the possibility of conception and when up to 80% of pathological gametes are detected in the spermogram.

In this case, attention is paid not only to the structure of the germ cells, but also to what is obtained when. This takes into account what is the ratio of the gametes of the pathological form to the total volume of the material obtained. If the examination of semen reveals a large number of cells with certain disorders, then the patient can be diagnosed with the following:
- Akinospermia is diagnosed when all the sperm in the ejaculate are immobile. Such gametes are unable to fertilize an egg. This is sterility.
- If the spermogram showed weak mobility of most cells, then they indicate the presence of asthenozoospermia.
- If, with the morphological characteristics of male sex cells, non-viable spermatozoa predominate, then this is necrospermia. It may or may not respond to treatment, that is, it is reversible or irreversible. In the latter case, the man is not able to have offspring.
- Teratozoospermia is characterized by the presence of a large number of structurally abnormal gametes. Such male germ cells are not capable of fertilization, since they simply cannot get inside the egg. But even if this becomes possible, it will lead to the formation of fetal pathologies or miscarriage.
It must be remembered that problems with conception can also arise if specific antibodies are present in the ejaculate. They are called antisperm. Such biologically active substances are produced and appear in the spermogram under the influence of various pathological processes, including inflammation or trauma. But they can appear for no apparent reason. Under their influence, various anomalies in the structure of spermatozoa can form, and their motor activity will decrease. In the most severe cases, the production of germ cells is suspended.
Not always, the pathology of germ cells in men can lead to complete infertility of the patient. The presence of abnormal structures in the ejaculate reduces the likelihood of natural conception, because such a gonad is simply not able to fertilize an egg. If the sperm has a pathology of the head, then it will not be able to penetrate into the egg. But even if this succeeds, an abnormal fetus develops. The process most often ends with an abortion.
If sperm cells are damaged in the tail or neck area, its mobility suffers. Such a gamete is simply not able to reach the egg. But this does not mean that natural conception is impossible. Indeed, even with serious abnormalities in the spermogram, the attending physician can offer modern medical methods of reproduction.
4 Informative value of Kruger analysis
Spermogram allows you to determine not all parameters of gametes. The most accurate characterization of their structure will allow a specific analysis of Kruger. What is its peculiarity? Why should a spermogram be combined with it? This study will help to identify the presence of morphological abnormalities in the structure of sperm and their ability to fertilize.
During the analysis, not only all cell structures are counted, but only healthy spermatozoa are taken into account. That is, those that have a regular oval head with a well-developed acrosome. Any deviations in the tail region or pathology of the sperm head are taken into account. A sperm capable of fertilization is considered one in which the number of pathologically unchanged cells will exceed 14%.
Based on the results obtained, the attending physician will determine the causes of the pathology of the structure of the sperm. Most often, this becomes an inflammatory process in the genital area and urinary system. Therefore, to eliminate violations in the spermogram and restore reproductive functions, anti-inflammatory therapy is performed.

The sperm produced in a man's testicles, with an increased number of them, do not all meet the necessary standards. A spermogram can help to determine how significant the pathology is, and in what it is determined. After determining the deviations and performing the correction of male infertility, which is caused by male poor-quality reproductive cells, the family will be able to replenish the baby.
Sperm quality assessment
Analyzes to identify the morphology of the spermogram are carried out in accordance with WHO and Kruger standards... The second way is tougher. It regulates that the number of perfectly healthy sperm in the examined sperm is limited to only 4%, and normally their number should be more than 14%. Any deviations are abnormal, this makes it possible to more accurately determine the fertility of a man.
If according to Kruger spermatozoa are assessed only in shape and appearance, then WHO determines the compliance of the source material with the norm only by the head.
But the sperm, in addition to this part, which makes up 11% of its total size, also has a body, which is attached by a neck and ends in a tail. At the same time, the tail accounts for about 75% of the total size. The head, with the nucleus in it, has an acrosome. With her sperm can dissolve the membrane in the egg and go inside. The translational movement creates a flagellum that makes rotational movements... Disruption of activity will entail the inability of the sperm to pass through the resistance of the vaginal fluid and reach the cervix, and then the fetal ovary.
Pathologies in the structure of sperm
Pathologies refer to all parts of the sperm. The following anomalies are distinguished:
Pathology can be in one of the above types or have a different combination of them. Not taken into account sperm without flagella, however, their presence is indicated in the spermogram.
Diagnosis
It is possible to determine a complete picture of the quality of sperm and its main component - spermatozoa - using a spermogram with Kruger morphology. Only this method makes it possible to determine the shape of the sperm, to find out how they move, how active they are, to observe their forward movement. The limit of mobility normally passes through the threshold of 32%.
In this case, the concentration of spermatozoa is determined. The spermogram reflects indicators of acidity and viscosity of ejaculate, its color, the volume of sperm secreted during a single ejaculation.
A spermogram is performed twice to prevent erroneous data; in some cases, a threefold repetition of the spermogram is performed.
As a supplement to the Kruger spermogram, a MAR test is prescribed, which supplements the picture with information on the presence of antisperm antibodies, and a semen examination is performed for compliance with WHO requirements. A positive result indicates that pathology is present.
 During the Kruger spermogram, sperm morphology is determined according to the scale developed by Kruger. This survey method is sperm analysis in full, and is the first step in the treatment and diagnosis of male infertility. Deciphering the results is rather complicated, which is why it is performed only by a specialist - reproductologist.
During the Kruger spermogram, sperm morphology is determined according to the scale developed by Kruger. This survey method is sperm analysis in full, and is the first step in the treatment and diagnosis of male infertility. Deciphering the results is rather complicated, which is why it is performed only by a specialist - reproductologist.
Preparation is required before analysis. It consists in abstaining from sex for several days. You also need to give up alcoholic beverages and go to the bathhouse. If you abstain from ejaculation for just one day, this will lead to the fact that the semen volume will be very small for analysis. If you abstain for more than 3 days, then the sperm will lose motility and the analysis will be incorrect. That is why it is necessary to abstain for exactly 2-3 days.
Testing method: masturbation. After ejaculation, it is necessary to collect the semen in a special container. Spermogram decoding is carried out only in the laboratory and implies revealing complete morphology... Then, when the analysis is submitted, and the transcript is on hand, the doctor conducts the treatment. The main objective of the treatment is to improve the quality of sperm, which is achieved by improving the morphology.
Decoding spermogram
Spermogram carefully examined with a microscope... The main emphasis is placed on such indicators of sperm:
- Sperm morphology. During the study of morphology, the structure and shape of the sperm itself is studied. Normal sperm must have slightly curled tails and oval heads.
- Mobility. During the calculation of this indicator, the number of sperm cells that move straight is determined. If the norms of mobility are found to be less than 32%, a disease such as asthenozoospermia can be considered.
- Quantity. Normally, there should be more than 15 million sperm in 1 ml of semen. When there are fewer of them, this indicates that a man has a disease such as oligozoospermia. If sperm are completely absent, then this is azoospermia.
Sperm that are abnormal are found in the semen of any man. Some have more, while others have less. But they have a major effect on reproductive functions. But during the presence of pathology in the reproductive cell of a man, she cannot fertilize a female egg... Also, during the presence of spermatozoa with pathologies in very large numbers, a huge obstacle appears to the movement of healthy spermatozoa. As a result, the impossibility of fertilization.
 Abnormal and normal sperm in a man can even be distinguished visually. A healthy sperm has a short neck, a slightly curled tail and an oval head. Normally, the head index should be 2.4 micrometers, the length ratio is 4-5 micrometers, the neck ratio: the size of the head multiplied by 1.5.
Abnormal and normal sperm in a man can even be distinguished visually. A healthy sperm has a short neck, a slightly curled tail and an oval head. Normally, the head index should be 2.4 micrometers, the length ratio is 4-5 micrometers, the neck ratio: the size of the head multiplied by 1.5.
An abnormal sperm at the end of the head may have abnormal forms of chromatin and incorrect location of the acrosome. Sometimes, during examination under a microscope, it can be seen that the acrosome is completely absent on the head, this indicates the presence of such a disease as globozoospermia.
Sometimes a loose attachment of the tail to the head can occur, as a result, this can lead to the separation of the tail. In this case, when examined with a microscope, only tails can be seen.
Establishing the correct diagnosis is possible only with a competent decoding of all pathologies present. That is why it is so important to contact only qualified specialists. Otherwise, some pathology will not be detected. Also, spermogram disorders allow calculate abnormal sperm index.
Until recently, only one anomaly index was determined - the number of spermatozoa with deformation in the structure of the head. Today it has become possible to determine the anomaly index not only on the head, but also on the neck and tail. The index has numbers from 1 to 3. Index 1 corresponds to the anomaly on the head only. Index 3 - the presence of abnormalities in all parts of the sperm.
Types of pathologies
An increased sperm count, with an existing pathology, in contrast to the norm, is called teratozoospermia. Its result is complete or partial infertility. The translational movement to the ovary and its fertilization with a sperm with different disorders creates a high probability that the pregnancy will pass with complications, and the newborn will have different defects. In the most severe case, the disease threatens a frozen pregnancy or miscarriage.
Disrupted sperm during teratozoospermia should be more than 70%... As a rule, this disease is accompanied by oligozoospermia and asthenozoospermia - a low concentration of sperm in the seminal fluid. The latter pathology is explained by the fact that the forward movement of the sperm is reduced, and it must be fast to get to the ovary. Only a small number of sperm cells are observed, which are actively moving.
During akinozoospermia, the movement of spermatozoa approaches zero, but their static character is temporary. During the examination, a revitalization procedure is used. If translational movement is not resumed, then sperm viability assessment.
Causes
 During the definition of the disease, it is necessary to determine the causes that caused it. They are congenital or caused by external causes. Teratozoospermia is usually associated with the constant presence in the zone of high temperatures, high radioactive radiation, other external factors, the accumulation of toxins in the body.
During the definition of the disease, it is necessary to determine the causes that caused it. They are congenital or caused by external causes. Teratozoospermia is usually associated with the constant presence in the zone of high temperatures, high radioactive radiation, other external factors, the accumulation of toxins in the body.
Infectious and inflammatory diseases of the genitourinary system have a negative effect, especially those that relate to the testicles and their appendages. Epididymitis, orchitis and their combination- orchiepididymitis - in the chronic stage, they cause significant damage to the quality of sperm. Infection occurs through blood or sexually.
Varicose veins of the testicle (varicocele) can lead to stagnation of blood, which ends with atrophy.
Men need to pay attention to their lifestyle and health. Conflict and stressful situations are also among the reasons.
Treatment
 Before starting treatment, a man will need to carry out andrological complex study including:
Before starting treatment, a man will need to carry out andrological complex study including:
- blood analysis;
- bacterioscopic semen analysis;
- Ultrasound of the scrotum and prostate.
The primary task of treatment is to eliminate the causes and factors as a result of which the pathology developed.
To improve the quality of ejaculate, it is necessary to eliminate stagnation in the small pelvis. These phenomena can appear with a sedentary lifestyle. To restore spermatogenesis, it is necessary to lead a healthy and active lifestyle, to exclude addictions and habits... Activities such as walking, swimming, running are useful. One of the main factors of treatment is the normalization of nutrition.
A man's menu must include a large amount of trace elements and vitamins, with the help of which the quality of ejaculate will improve. A man will have to forget about fatty foods. Typically, his meals will consist of seafood, fish, fresh fruits, legumes, grains, and crops. In addition to vitamins, dietary supplements can also be prescribed.
Male infertility, developed due to morphological disorders of spermatozoa, may require treatment with additional reproductive technologies. These technologies significantly increase the chances of a couple to conceive a child, as well as to give birth to him healthy.
If there are small deviations, then an artificial insemination method may be recommended. Before the procedure, sperm is taken from the man, which undergoes special processing, as a result, in the sperm the quality of sperm increases.
 When the semen contains an unnecessarily high number of abnormal sperm cells, in vitro fertilization, which is performed with the help of assisted procedures, will be a more effective treatment option. With these methods, only healthy and mature sperm can be selected from all sperm, thereby reducing the risk of abnormal fetal development and miscarriage.
When the semen contains an unnecessarily high number of abnormal sperm cells, in vitro fertilization, which is performed with the help of assisted procedures, will be a more effective treatment option. With these methods, only healthy and mature sperm can be selected from all sperm, thereby reducing the risk of abnormal fetal development and miscarriage.
Modern methods of treatment in combination with an active and healthy lifestyle, as well as proper nutrition can save a man from infertility and improve the quality of sperm morphology. It is very important not to panic during the detection of pathology in the structure of sperm cells, but to consult a doctor as soon as possible, follow all his recommendations and certainly believe in yourself.
A condition in which the semen contains a large number of sperm with structural abnormalities is called teratozoospermia. The pathology of the sperm head in the spermogram is detected much more often than other abnormalities and is considered the most severe disorder due to the increased risk of miscarriages and freezing of pregnancy in the early stages. Basically, such a pathology is provoked by infections and hormonal disruptions in a man's body.
The main indicators of the normal and pathological structure of the sperm head
The sperm head without structural abnormalities has the following characteristics:
- oval shape;
- smooth surface;
- length 3-5 mm;
- width 2-3 mm;
- lack of vacuole cells;
- clear selection of the acrosome (apical body).
The pathology of the sperm head is detected if:
Our regular reader got rid of problems with potency with an effective method. He tested it on himself - the result is 100% - complete elimination of problems. It is a natural herbal remedy. We have tested the method and decided to recommend it to you. The result is fast. EFFECTIVE METHOD.

- the head has an abnormal shape (round or conical);
- the head has non-standard dimensions (too large or too small);
- the sperm has multiple heads;
- acrosome occupies less than 40% of the head or is absent;
- vacuoles are present in the head.
Causes of the pathology of the sperm head
Pathological forms of sperm are present in the spermogram of every man. A deviation from the norm is the condition when the number of morphologically abnormal cells exceeds the number of healthy sperm.
Among the main causes of defects in the sperm head are:
- bacteriological infectious diseases (chlamydia, gonorrhea, mycoplasmosis);
- viral infections (mumps, herpes);
- hormonal disruptions in the body;
- the presence of inflammatory processes in the genitals (prostatitis, inflammation of the epididymis, inflammation of the testicle, thrush);
- tumors, cysts;
- varicose veins of the spermatic cord and testicle;
- endocrine disorders (diabetes mellitus);
- diseases of a genetic nature;
- genital trauma;
- alcohol abuse, smoking;
- frequent stress and overwork;
- improper nutrition;
- negative impacts environment(radiation, thermal effects).

Only full-fledged sperm are able to get to the fallopian tubes and fertilize an egg
How sperm head abnormality affects fertility
For natural fertilization to occur, healthy sperm in the semen (2-2.5 ml) must be at least 15-20 million. Only full-fledged spermatozoa are able to overcome the acidic environment of the vagina, get to the fallopian tubes and fertilize the egg. If there are not enough cells without abnormalities in the ejaculate, fertilization can be significantly hampered - two-headed spermatozoa or sperm with non-standard head sizes will not be able to penetrate the membrane of the female reproductive cell. The likelihood of a natural pregnancy and the chances of having a healthy baby in this case are very small. Often teratozoospermia is characterized by early pregnancy fading or miscarriages. To avoid unpleasant consequences, married couples wishing to have a child should abandon conception planning until normal test results are obtained.
Diagnosis of the disease
Teratozoospermia is diagnosed only after conducting a study of the analysis of the ejaculate - spermogram. This is the very first analysis that is assigned to a man with a problem of infertility.
To diagnose pathologies, sperm cells are examined by immobilizing them in advance in a special counting chamber. The diagnosis is made if the concentration of sperm with abnormal structure exceeds 85%. To determine (anomaly index), the number of abnormalities is divided by the number of cells with pathology. With the help of this indicator, a forecast of a man's fertility is made and the possibility of conception is determined using artificial insemination methods.
The indicators may change slightly, so after a few days the analysis of the man needs to be repeated. Doctors advise in two different laboratories so that the result is as accurate as possible.

After the examination, the man is prescribed treatment by a doctor - andrologist
Treatment
After the examination, the man is prescribed treatment by a doctor - andrologist. Treatment of the pathology of the structure of the sperm depends on the causes of the disease. For example, if the violation provoked an inflammatory process, the doctor prescribes special anti-inflammatory drugs to the patient, and if infectious diseases the man is shown viral and antibiotic therapy. In case of disorders of the endocrine system, an endocrinologist's consultation is prescribed, followed by treatment, which normalizes the hormonal background. The help of a psychotherapist is necessary for pathology caused by stressful situations. If the cause of teratozoospermia is obstruction of the vas deferens, the patient is shown surgery... If the problem lies in the wrong lifestyle and harmful external influences, it will be advisable to reduce the influence of negative factors.
In addition to drugs that help eliminate the causes of the disease, a man is recommended to take additional drugs that improve the quality and quantity of sperm. Among them are folic acid, selenium, zinc, iodomarin, L-carnitine and vitamin E.
For the treatment of pathology using folk remedies, you can try eating porridge, mashed potatoes, honey, nuts and dried fruits. Among the drinks, the most useful are pumpkin juice and herbal tea.
The treatment prescribed by a specialist should be carried out for six months. In case of an untimely visit to the doctor and in advanced cases, the patient is recommended the IVF program. With careful selection of normal sperm for fertilization, the risk of termination of pregnancy and the development of fetal defects is minimized.

Among the methods of artificial insemination, in vitro fertilization is distinguished.
IVF and artificial insemination in teratozoospermia
The likelihood of a natural conception of a child from a man with a pathology of the sperm head is small, therefore, methods of artificial insemination can come to the aid of a married couple. These methods include in vitro fertilization (IVF) and artificial (intrauterine) insemination.
The IVF procedure is a common and approved method by all specialists. For IVF required amount sperm cells and an egg are placed in a special container in order for fertilization to occur. Then the embryo is placed in the woman's uterus and, if the procedure is positive, the fetus develops.
The main advantage of IVF is that only cells without structural disturbances are selected from a large number of sperm. Although there are few full-fledged sperm with teratozoospermia in the ejaculate, they are still there in one or another quantity. It is these full-fledged cells that are subsequently used for fertilization. Provided the woman's attitude to pregnancy is correct, the fetus developing as a result of IVF will have absolutely no abnormalities.
If the method of intrauterine insemination is used, then a sufficiently prepared sperm is injected into the woman's uterus through a catheter. This method is suitable for a married couple if a man is diagnosed with a mild degree of teratozoospermia, and spermatozoa with a pathology of the head structure are present in the ejaculate in small quantities. In this case, the sperm only need help to get to the uterus. Intrauterine insemination shortens this distance, resulting in pregnancy.
Since the pathology of the sperm head is often provoked by an incorrect lifestyle, a man should also adjust his diet, give up bad habits and pay attention to normalize weight. The effect of any medication will be more effective if you try to avoid stressful situations during treatment. With a timely appeal to a specialist for the appointment of treatment and with the right approach to your lifestyle, the results of a spermogram can significantly approach the norm.
Are you having serious POTENTIAL problems?
Have you tried a lot of tools and nothing helped? These symptoms are familiar to you firsthand:
- sluggish erection;
- lack of desire;
- sexual dysfunction.
Pathological forms in the spermogram can be detected for various reasons. A spermogram is a semen analysis that is prescribed to establish a man's ability to fertilize or identify diseases of the genital area.
Collapse
A spermogram is prescribed for a man if:
- a married couple complains of infertility;
- the man is a sperm donor;
- before cryopreservation (freezing) of sperm.
The analysis is carried out in laboratory conditions under a microscope. The number of spermatozoa, their external structure, the level of leukocytes, etc. are examined. The volume of ejaculate, color, sperm viscosity, pH of the medium (degree of acidification or alkalization) are also taken into account.
Over time, ideas about the rate of ejaculate changed. Currently, there are no established norms, sperm fertility is determined by the general ability to fertilize. WHO has proposed guidelines for the study of human ejaculate that are highly regarded by physicians. It proposes norms and rules for conducting a spermogram.
The more healthy male cells in the external structure, the higher the objective possibility of a successful conception. However, if pathologies are present in the test material, this is a direct path to male infertility. An altered, unhealthy form of the male reproductive cell is called teratozoospermia.
What is meant by the term "sperm pathology"?
During the microscopic examination (spermogram), the main parameters of the sperm are studied: the structure of the head, middle part and tail. Violations during external structure sperm cells are considered a pathology. For example, an asymmetrical head shape, a too thin or thick middle part of a male cell, a long or short tail, etc.
The pathology of the shape of the head can look like pear-shaped, conical, large, small, double. The position of the head may be incorrect.
The pathology of the shape of the middle part - the neck - is always an incorrect attachment to the head.

Tail pathology is a very long or, conversely, a short tail, double, wide. All this prevents the male cell from moving normally in order to reach its goal - the egg.
The required norm of healthy male cells is considered to be 4%. A smaller number refers to pathology, because the likelihood of conception decreases, and if it does occur, then the risk of miscarriage or congenital diseases in the fetus is high.
In the spermogram, you can still find such terms as "asthenozoospermia" and "oligozoospermia". The term "asthenozoospermia" means that the motor ability of male cells is below the prescribed level. And oligozoospermia is a small number of male germ cells.
The pathological forms in the spermogram also include sperm in which there are no male cells. The medical term for this is azoospermia.
Spermagglutination is a term that refers to the attachment of sperm to each other. The main reason for this pathology is the presence of antisperm antibodies (ASAT). They oppose their own male cells and prevent them from joining the egg.

Sperm aggregation is also the adhesion of spermatozoa that occurs due to the excess amount of mucus in the ejaculate. The nature of this cell adhesion differs from spermagglutination.
In the study of pathological forms in the spermogram, in addition to external signs, sperm cells are also examined for viability. A motile sperm cell is considered the norm. If he does not move, then he is either dead, or his motor functions are impaired. However, if 50% of the total number of ejaculate is live and motile sperm, then this sperm is not considered unhealthy.
In order to determine whether a sperm is a pathological form, the eosin staining method is used. The essence of this method is that eosin (dye) cannot penetrate into the living sperm. If this happens, then he is dead. The more colored sperm there are in the semen, the more unsuitable for fertilization.

The next way to determine the number of pathological forms is a hypoosmotic test. Spermatozoa are immersed in a special solution and kept in it for about 2 hours. Living, or suitable, spermatozoa swell in solution, while dead ones do not change.
The number of leukocytes in the ejaculate can tell a lot. Their increased number indicates the presence of a disease, due to which there is a change in the shape of the sperm.
Sperm motility is also affected by the ability of the ejaculate to liquefy. Normally, this should happen within an hour. If the sperm does not liquefy, then the possibility of conception drops sharply. This is a pathology of the prostate gland. The organ must produce a certain amount of enzymes that reduce the viscosity of the semen.

Semen color is not particularly important during semen analysis. But if the sperm has a pink or brown tint, then this may be a sign of the presence of blood in it. This may be due to a genital infection, inflammation, or swelling.
There are many reasons for this problem. They can be both diseases and the impact of the external environment. Let us consider in more detail the factors that can cause the pathology of human ejaculate.
Diseases of the male genital organs:
- prostatitis, urethritis;
- genital infections;
- viral infections such as mumps (mumps);
- varicocele - a pathology of the vessels of the penis;
- tumors.

Impact of external factors:
- radiation;
- excessive warmth;
- poor nutrition.
Hormonal Disorders:
- endocrine system diseases;
- a decrease in the amount of male hormones against the background of an increase in female hormones.
Impact of bad habits:
- smoking;
- alcohol;
- drugs;
- overwork;
- stress;
- insomnia;
- taking anabolic steroids;
- genetic predisposition.
Terms found in semen analysis:
- Normospermia - indicators are normal.
- Teratozoospermia - the number of sperm with defects in the structure exceeds the level of normal cells.
- Asthenozoospermia - sperm are inactive.
- Oligozoospermia is a small amount of sperm.
- Azoospermia - there are no sperm in the ejaculate.
Male ejaculate, or semen, is considered normal if it contains a small amount of abnormal sperm. The main thing is that their number does not exceed the norm and does not interfere with healthy cells.
Abnormal sex cells include sperm with defects in the head, neck or tail. They can no longer fertilize an egg or become the cause of pregnancy pathology.
The number of healthy forms of sperm is assessed according to the Kruger criteria. Normal cell forms must be at least 50% for successful fertilization. Very often it is defective sperm cells that cause male infertility.
The higher the level of defective sperm in the ejaculate, the greater the likelihood of infertility or missed pregnancies. Teratozoospermia occurs for several reasons, including diseases of the testicles and epididymis.
Decoding spermogram
Spermogram is a diagnostic procedure that allows you to determine the quantitative and qualitative parameters of the ejaculate.
The study is shown in such cases:
- the inability to conceive naturally;
- planning pregnancy, in order to assess the reproductive health of a couple;
- prospective donation, IVF.
A spermogram can reveal defective germ cells in a healthy man, a high percentage of which affects the possibility of conception. It is considered a pathology when defective sperm cells exceed 50%.
Fertility and defective germ cells
 The following factors can affect the sperm defectiveness index:
The following factors can affect the sperm defectiveness index:
- pathology of the testicles and their appendages, including inflammatory and non-inflammatory diseases, parotitis;
- bacterial and viral sexually transmitted infections;
- benign and malignant formations;
- negative thermal effects, radiation, unbalanced nutrition;
- endocrine diseases, a decrease in the level of male hormones;
- genetic abnormalities, bad habits and unhealthy lifestyles.
Teratozoospermia is quite often diagnosed against the background of pathology of the sperm head. Changes such as defect in size, quantity, shape may be observed. There may also be an asymmetry of the attachment of the neck and the middle part of the sperm, or it may have an uneven, short tail. All of these abnormalities affect male fertility, reducing the possibility of egg fertilization.
Causes of head defect
Sperm defectiveness can be triggered by the following factors:

There are various forms of teratozoospermia:
- Head defect. It can be reshaped and have an asymmetrical acrosome.
- Midsection and neck defect. The thickness, the angle of inclination may be violated.
- Tail defect. It can be short, multiple, oblique.
Treatment
Teratozoospermia does not have a specific treatment regimen. First of all, it is necessary to eliminate the cause of the bad spermogram. The formation of defective spermatozoa may be associated with inflammatory processes of the genital organs, then anti-inflammatory therapy is prescribed.
 In case of hormonal imbalance in a man's body, hormonal treatment is prescribed. If the cause is varicocele, a surgical procedure is performed, during which varicose veins of the testicles are eliminated. In most cases, such treatment eliminates the causes of teratozoospermia and the male's sexual health is restored.
In case of hormonal imbalance in a man's body, hormonal treatment is prescribed. If the cause is varicocele, a surgical procedure is performed, during which varicose veins of the testicles are eliminated. In most cases, such treatment eliminates the causes of teratozoospermia and the male's sexual health is restored.
In addition to etiological treatment, it is important for a man to take drugs that contain a specific amino acid and macronutrients. Strengthening the immune system and special nutrition, including foods rich in zinc, selenium, iodine and folic acid, can prevent the formation of cells with head pathology.
Honey and bee pollen will be useful in this case, which should be eaten half a teaspoon daily. For the period of restoration of fertility, a man must give up bad habits, eliminate stressful situations, as well as heavy physical exertion and work in hazardous industries. In rare cases, defects in the head of the sex cells cannot be eliminated medically or surgically, then the doctor recommends the couple to resort to artificial insemination.
Teratozoospermia can also occur due to toxic poisoning. In this case, the body is detoxified, at the same time the man must exclude alcohol and drugs.
Malignant and benign formations that have caused a defect in the sperm head are treated together with an oncologist and other specialized doctors.
It also happens that teratozoospermia occurs due to an unexplained etiology, then it is almost impossible to eliminate it. In this case, they resort to specific treatment, L-kartynin, amber and folic acid, Iodomarin, vitamin E, Spermoactin drug.
Folk remedies for head pathology
 Self-medication for teratozoospermia is excluded, no folk remedies cannot lead to the restoration of the male reproductive function and affect the defect of the sperm head. All existing recipes can be used in parallel with medication or surgical treatment for the purpose of general strengthening of the body.
Self-medication for teratozoospermia is excluded, no folk remedies cannot lead to the restoration of the male reproductive function and affect the defect of the sperm head. All existing recipes can be used in parallel with medication or surgical treatment for the purpose of general strengthening of the body.
During treatment, the pathology of the sperm head is recommended for men to drink green tea, brew currants, since it is rich in vitamin B9 and ascorbic acid... These substances contribute to the production of normal germ cells. You can drink 200 ml of currant tea daily, with the addition of a spoonful of sugar or honey.
It is also good to eat pumpkin dishes. It can be porridge, puree or dried fruit. Pumpkin juice is no less useful, which can be consumed in any quantity without harm to health. Doctors also confirm the benefits of a decoction of birch leaves, nettle, plantain seeds. It can be taken in 250 ml daily.
Nutrition for sperm pathology
A man's nutrition in the presence of a defect in the sperm head is focused on the restoration of vitamin B9 in the body.
With teratozoospermia, it is useful to use the following foods:
- walnuts, broccoli, carrots, cabbage;
- greens, asparagus, parsley, spinach;
- lamb, chicken, beef;
- flour and cereals of coarse grinding.
Sperm defect diagnosis
 For treatment to be effective, it is not enough to identify defects in the sperm head. It is necessary to find out the cause and accompanying deviations, and for this there are several basic and additional diagnostic measures.
For treatment to be effective, it is not enough to identify defects in the sperm head. It is necessary to find out the cause and accompanying deviations, and for this there are several basic and additional diagnostic measures.
Spermogram is the main test that allows you to determine the amount of semen and the concentration of sperm. This method examines the mobility, morphology and percentage of normal germ cells. The test can also detect signs of inflammation, pH, oxygen particles, and round cells.
The spermogram also has a minus, since during the study it is impossible to identify some deviations that have caused infertility and defective sperm.
Additional tests include:
- autoimmune test - allows you to determine the presence of antibodies in sperm, which interfere with their attachment to the egg;
- to determine the functionality of germ cells, sperm cells are analyzed with washing, which makes it possible to determine the level of cell motility;
- a test for the viability of germ cells shows the potential of sperm to fertilize;
- halo test allows you to identify sperm with DNA breaks;
- SDI test - similar to the previous study, but more informative.
High-quality diagnostics is an integral part in the process of identifying and eliminating sperm defects. Some men have been struggling with a problem for years only because the root cause has not been identified for a long time.
Topic: Potency like at 18!
From: Mikhail P. ( [email protected])
To: Administration http: // site
Hello! My name is
Mikhail, I want to express my gratitude to you and your site.
Finally, I was able to establish potency. I have an active sex life, my relationship with my wife has reached a new level!
And here is my story
From the age of 35, due to a sedentary and sedentary lifestyle, the first problems with potency began, "I was only enough for 1 time," the duration and quality of sex decreased significantly. When I turned 38, real problems began, I began to panic, and in order to somehow improve my sex life I began to resort to Viagra and its analogues. And the pills seemed to "work", but later I realized that without the pills the erection was gone completely! And Viagra is quite expensive, and besides, it has a huge amount side effects, which have an extremely negative effect on the entire body. All this led to constant quarrels with my wife, I was on the verge of a nervous breakdown, everything was very bad ...
Everything changed when a friend at work advised me one remedy. You cannot imagine how much I am grateful to him for that. I only drank 2 tablets a day and had sex for 2-3 hours every day! In addition, after drinking just one course, my potency fully recovered, and became more powerful than at 18 years old without any pills! The result has been lasting for 2 years! Most importantly, relations in the family have improved. My wife and I are just happy.
It doesn't matter if you have the first symptoms or have been suffering from poor potency for a long time, I advise you to drink the course of this remedy, I guarantee you will not regret it.
How to help yourself with folk methods
There is a mass healthy recipes that qualitatively affect spermatogenesis. For starters, it is recommended to replace regular black, green tea with herbal tea. You can prepare it from currant leaves. They contain vitamin B9, which directly affects the production of sperm. You need to drink such brewed tea 3-4 times a day for a month.
Also, pumpkin porridge contributes to the normalization of sperm. Pumpkin juice is often used. Fresh juices can be done several times a day (2-4 times). Decoctions of nettle and birch are considered miraculous. Leaves of plants are taken in equal amounts and steamed for 20-25 minutes. This broth must be drunk for two weeks.
Conclusion
Traditional methods should not be basic, but can be supported by drug treatment. If the pathology of the head carries a genetic abnormality, it is impossible to cure infertility. In this case, the couple may be advised to undergo IVF. With artificial insemination, only healthy and strong sperm are taken from men, which are then implanted into the egg. According to statistics, in 78% of cases, head pathology is treated successfully by eliminating the root cause of sperm deformation.
Usually, when a man ejaculates, from 2 to 10 ml of sperm is released - its volume depends on the frequency of sexual intercourse, constitution, emotional state and other factors. In a healthy man, 1 ml of ejaculate contains 60-120 million sperm. In addition to the spermatozoa themselves, it contains spermatogonia and spermatids, sperm precursor cells. Among the non-cellular elements, lecithin bodies, prostatic crystals, pigment grains, and fatty inclusions are distinguished. The secretion of the prostate gland dilutes the ejaculate; together with the secretion of the seminal vesicles, they form a favorable breeding ground for sperm.
Sperm morphology abnormalities
In the spermogram of a healthy man, along with normal sperm forms, there are also pathological forms of sperm, but no more than 20-25%. Exceeding this number can lead to infertility or to congenital malformations of the fetus. With pathology in the ejaculate, the number of normal spermatozoa decreases and the number of motile forms may decrease.
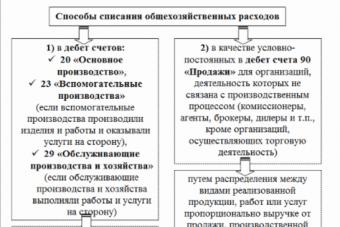
Absent (spermatozoa are normal or with mild pathology) - tail pathology - acrosome abnormalities (decrease in size, absence) - change in the shape of the nucleus - immature forms (with a cytoplasmic drop) - pathology of the neck and midline - doubling or change in the head section
Sperm tail pathologies affect their mobility (they have impaired movement or are completely motionless). Acrosome abnormalities affect the sperm's ability to fertilize an egg. An increase in the ejaculate of cells with nuclear pathology may be associated with a deterioration in the morphology of embryos and, as a result, with a decrease in the frequency of pregnancy. The presence of spermatozoa with a cytoplasmic droplet may indicate a violation of the sperm maturation process. Anomalies of the neck and midline, as well as changes in the size and doubling of the head, as a rule, are recorded last.
Major sperm pathologies
AZOOSPERMIA (a ... + zoo ... + sperm), the absence of spermatozoa in the ejaculate, but the presence of the preceding forms - spermatogenesis cells along with the secretion products of the prostate gland and seminal vesicles. It should be distinguished from aspermia. With azoospermia, spermatogenesis (division or maturation of spermatozoa) is inhibited at various stages. This can be caused by congenital (genetic) disorders, toxic effects (radiation, alcohol, harmful chemicals, some drugs, etc.), various diseases of the body. Various types of violations of the patency of the vas deferens as a result of inflammatory diseases of the genital organs can also lead to azoospermia. Azoospermia is one of the causes of infertility in men, which requires examination and treatment by a doctor.
AQUINOSPERMIA (I ... + Greek. Kineo- set in motion + sperm; synonym- akinesia), complete immobility of living sperm in sperm and their inability to fertilize.
The reasons for this phenomenon are not well understood. Presumably, they can be diseases of the gonads (most often inflammatory), hormonal deficiency, etc.; in laboratory conditions - sharp hypothermia of sperm during storage, illumination of it with direct sunlight, accidental ingestion into a test tube with sperm chemical substances, obtaining sperm in a condom, etc. When establishing akinospermia, a 2-3-fold thorough examination of the ejaculate is necessary (see spermogram).
ASPERMIA (a ... + sperm), absence of spermatozoa and spermatogenesis cells in the ejaculate At the same time, during intercourse, the secretion of fluid, consisting of the secretion of the prostate gland, seminal vesicles, and the sensation of orgasm are preserved, which distinguishes aspermia from aspermatism However, the amount of fluid released during ejaculation , very insignificantly, and the sensation of orgasm is poorly expressed and erased. The cause of aspermia is the congenital absence or underdevelopment of the vas deferens or their blockage due to inflammation or trauma to the genital organs (obstructive aspermia), as well as the inability of the testes to produce sperm (testicular aspermia). Testicular aspermia is a sign of secretory infertility as a result of genetic gender abnormalities. In such cases, treatment is futile. Aspermia due to blockage of the vas deferens is the cause of excretory infertility and requires plastic surgery.
ASTENOZOOSPERMIA (Greek asthe neia - powerlessness, weakness + zoo ... + sperm; synonym - asthenospermia), a decrease in the number of mobile forms, as well as the speed of movement of sperm in semen. The number of inactive or immobile forms in this case exceeds 30%. The causes of asthenozoospermia are not fully understood, but the role of the change is assumed chemical composition sperm plasma, a decrease in the content of carbohydrates or other energetic substances in it, as well as a decrease or disappearance of the negative electric charge of sperm, deposition of various microorganisms on their surface, especially mycoplasma infection. The reason may be various disorders of spermatogenesis, as a result of which not only a smaller number of spermatozoa (oligozoospermia) is formed, but also pathological, abnormal forms (teratozoospermia), incapable of full-fledged movement. Asthenozoospermia can lead to infertility in men, which requires consultation with a urologist, medical examination and treatment.
HEMOSPERMIA (Greek haima, haimatos - blood + semen), the appearance of blood (erythrocytes) in the semen, which at the same time acquires a red or "rusty" color. Most often, blood enters the sperm from the seminal vesicles or prostate in their inflammatory or tumor diseases. Blood can also appear in the ejaculate from the urethra, vas deferens or epididymis, in the presence of stones in the prostate gland, rupture of small varicose veins, papillomas, seminal tubercle and for other reasons. Hemospermia does not reduce sperm viability, but indicates a disease of the genitals, which makes necessary carrying out urological examination to establish the source of bleeding and appropriate treatment.
HYPOSPERMIA (hyp ... + sperm), see Oligospermia.
NECROSPERMIA (necr ... + semen), the presence of non-viable sperm in the ejaculate. Necrospermia is reversible (false), when the revival of sperm is successful, and irreversible (true). The latter is extremely rare, its causes have not been clarified and it cannot be treated. There is also partial necrospermia, in which living sperm is less than 20%. Necrospermia due to immobility of spermatozoa is often mistaken for akinospermia.
The phenomenon of necrosperm is sometimes attributed to the effect of the dye on sperm or the accidental ingress of chemicals into a test tube with sperm during its examination. Samples are taken repeatedly to avoid artifacts. In cases of true necrospermia, childless spouses should be advised artificial insemination sperm donor or adoption. False and partial necrospermia, which can be caused by asthenozoospermia, akinesia and other factors, is amenable to drug treatment.
NORMOSPERMIA (norm ... + sperm; synonym - normozoospermia), a state of the body in which all spermogram indicators are within normal values. The content of spermatozoa in the ejaculate in a healthy mature man is 60-150 million / ml, of which at least 70% are mobile. Normospermia indicates a normal spermatogenesis process and high sperm viability. However, the latter does not guarantee 100% pregnancy in a gynecologically healthy woman. The reasons for possible infertility can be psychological, often unconscious or inexplicable due to insufficient development of knowledge at the moment.
OLIGOZOOSPERMIA (olig ... + zoo ... + + sperm), a decrease in the number of sperm in the ejaculate. It should be distinguished from oligospermia.
Sperm is considered normal if 1 ml contains 60-150 million sperm (see Normospermia).
There are several degrees of oligozoospermia: I - 1 ml of ejaculate contains 60-40 million sperm; II-40-20 million; Ill-20-5 million; IV - less than 5 million. Currently, the lower limit of the norm has been revised and according to the World Health Organization (WHO) is 20 million sperm in 1 ml of ejaculate. It is believed that for the onset of pregnancy, this amount of sperm may be sufficient, provided their normal amount is 2-5 ml of ejaculate and a high fertilizing capacity. It is only necessary that a certain amount of sperm enter the uterus to the egg, the so-called "fertile pool", which will create the conditions for the penetration of one sperm into the egg and its fertilization. If pregnancy does not occur in a healthy examined woman, then oligozoospermia, regardless of the degree, should be considered as a pathological condition. The causes of oligozoospermia are considered hormonal deficiency, leading to impaired spermatogenesis, starvation, vitamin deficiency, alcohol and nicotine abuse, chronic poisoning with lead, mercury and their derivatives, carbon dioxide, the action of X-ray and radioactive radiation, chronic inflammatory processes (chlamydia, other mycoplasmosis). Physical and mental overwork, stress, conflicts, as well as frequent ejaculation in any form (intercourse, masturbation, emissions) can lead to oligozoospermia. A healthy person is also characterized by fluctuations in the number of sperm, but they do not exceed 10-15% in one direction or another. Deciding whether oligozoospermia is the cause of infertility is within the competence of the physician.
OLIGOSPERMIA (olmg ... + sperm; synonyms - hypospermia, hypovolumia), a decrease in the volume of ejaculate ejected during ejaculation. It should be distinguished from oligozoospermia.
The volume of ejaculate usually does not exceed 1-1.5 ml, while the norm is 2-5 ml. The most common causes of oligospermia are hormonal deficiency, various congenital, genetic diseases (for example, Klinefelter's syndrome), aspermia and azoospermia, chronic prostatitis of various origins, mental fatigue, conflicts, alcohol, and poor nutrition. Oligospermia can also occur in healthy men with too frequent sexual intercourse or masturbation. Therefore, one can speak of true oligospermia only if the man, before receiving sperm for analysis, refrained from any form of ejaculation (intercourse, masturbation, emission) for 4-5 days and collected it without loss in laboratory glassware. Those suffering from oligospermia, like other disorders of spermatogenesis, should seek the advice of a doctor.
PIOSPERMIA (Greek ruon - pus + semen), the presence of pus in the semen. The semen at the same time has a greenish-yellow color and often a fetid odor. It contains leukocytes, microorganisms, decaying cells, etc. Pyospermia is often combined with hemospermia, oligospermia, teratozoospermia.
Sources of pus can be any part of the genital organs, but more often the urethra, seminal vesicles, epididymis, prostate gland.
Toxins (toxic substances) secreted by microorganisms have a damaging effect on spermatozoa, increasing the number of pathological forms and disrupting sperm motility, which naturally reduces the fertilizing ability of sperm. Pyospermia is always a sign of an inflammatory process in the male genital area, which requires urological examination and treatment.
POLYSPERMIA (poly ... + sperm; synonyms - multisemia, multipole), persistent discharge during ejaculation of an increased number of sperm in the ejaculate (over 250-300 million / ml). Sometimes the term "polyspermia" is used to refer to a large volume of ejaculate - more than 8-10 ml. Moreover, all spermogram indicators are within normal limits. It is believed that the cause of this condition is a violation of spermatogenesis.
The increased spermatogenetic activity of the seminiferous tubules of the testicles leads to the appearance of spermatozoa with low fertilizing capacity. Quite often, with the husband's polyspermia, a woman may have miscarriages or no pregnancy. For the purpose of conception, it is recommended to dilute sperm with special solutions and artificially introduce it into the uterus for the purpose of insemination. The medical tactics for treating male infertility with polyspermia is not clearly defined.
TERATOZOOSPERMIA (Greek teras, teratos-freak, deformity + zoo ... + sperm; synonyms - teratospermia, anisozoospermia), the presence of pathological, abnormal forms of spermatozoa in the ejaculate in an amount exceeding 50%. The causes of teratozoospermia are the same as in oligozoospermia and asthenozoospermia - pathological conditions or unfavorable environmental factors leading to impaired spermatogenesis.
According to some data, artificial insemination with sperm with a large amount of degenerative sperm in 45-65% of cases entails severe fetal development disorders, often the cause of miscarriage, miscarriages. If the ejaculate contains a large number of pathological forms of sperm, the spouses should temporarily refrain from conceiving, and the husband should undergo the necessary treatment from an andrologist.
Sperm can be significantly impaired by smoking, drinking alcohol, and improper diet. She is susceptible to various diseases, including sexually transmitted diseases. Therefore, before conceiving a child, it is advisable to undergo appropriate examinations and exclude pathologies, this can be done using a spermogram.
Patologija_spermy._osnovnye_terminy.txt · Last modified: 2012/06/21 22:58 (external change)